Fostering Hope and Coping While Living With Lymphedema: A Visual Narrative for Engaging Cancer Survivors and Caregivers
By Roanne Thomas, PhD, Ryan Hamilton, PhD, Gen Allen, Viviane Grandpierre, PhD, Josée Boulanger, Christine Novy, and Yvonne Anisimowicz
Introduction
Lymphedema is a chronic condition that affects approximately 5 million Americans.1,2 In developed countries, it has primarily been viewed as a secondary disease stemming from cancer and/or its treatments. Lymphedema typically results in painful limb swelling. It can impact psychological well-being—often due to poor perception of body image, for example1—and limit physical function in the affected limb leading to difficulty with everyday activities such as dressing and walking.3-7 In addition, lymphedema may lead to acute cellulitis—an infection that, without treatment, can become life-threatening.3
The psychosocial well-being of cancer survivors is often affected by the presence of lymphedema. Research has shown quality of life to be poorer among cancer survivors with lymphedema in comparison to those without.7 One aspect of well-being proven to be beneficial for cancer survivors is hope.8-10 Hope can ease despair and physical decline as well as increase positive life outlooks.11,12 Cancer survivors with lymphedema may also be advised to utilize various coping strategies to manage physical, psychological and social impairments of cancer. These strategies include problem-focused coping (i.e., practical strategies to eliminate or mitigate stressors) and emotion-focused coping (i.e., strategies to manage the emotional response to stress).13 Additionally, social support and resources, such as caregivers or practitioners, have assisted survivors in coping with the challenges caused by lymphedema.1,7,14 Such interventions have also been shown to increase awareness of treatment options as well as comprehension of hope and its relationship to coping.9,10
Our research program focuses on fostering hope and coping strategies for those living with lymphedema. As such, one of our goals was to create a video for people with this condition, as videos are an engaging and effective medium to raise awareness. Another goal was to increase health professionals’ knowledge about lymphedema and its impact on people’s lives. Video’s ability to mimic reality creates a feeling of intimacy, allowing viewers living with secondary lymphedema after cancer to connect with storytellers (ie, our participants) and, thereby, potentially reduce their sense of isolation. This may encourage viewers to seek further information and treatment as well as, at the very least, to begin to discuss with family and health professionals the challenges of living with lymphedema. Furthermore, video modelling suggests that viewers identify with those in the film and that this contributes both to improving well-being and changing behavior (eg, finding ways to foster hope and to cope in difficult situations).15 More specifically, video has assisted audiences with finding ways to generate hope in difficult situations.9,10,16
Creating the Video
The content in our video, Learning to Live with Lymphedema: ‘A New Me’, was informed by findings stemming from two studies associated with our program of research.17-20 In our first study, we conducted qualitative interviews with 13 participants from the provinces of New Brunswick and Ontario in Canada.17 These participants were living with upper- or lower-limb lymphedema secondary to cancer. Study 1 showed that those with secondary lymphedema after cancer must accommodate a number of losses, including but not limited to loss of function (e.g., leisure), maintaining a “normal” appearance while encountering stigma, and reduced productivity (e.g., at paid work).17 Participants indicated that psychosocial support would aid in lymphedema management, which is necessary because it is a “lifelong condition” to which they must adjust.17
In response to these findings, Study 2 included two pilot tests of a group-based intervention consisting of community-based workshops aimed at enhancing psychological coping skills and fostering hope.18-20 These workshops included creative projects where participants were invited to engage in either reflective writing or collage. The workshops were facilitated by a multidisciplinary team that included a psychologist, sociologist, occupational therapist, and physiotherapist. We described the interactive and participatory features of workshop facilitation in a recent publication.20
The Participants
Four participants, reflecting some diversity in experiences (e.g., gender, culture, age, and extremity involvement) were identified from Study 2 and invited to participate in the Learning to Live With Lymphedema: ‘A New Me’ video. Each agreed to share their stories via video. The video content directly reflects Study 1 interview themes as well as data analyzed from the transcripts of workshop recordings in Study 2. The team’s prior knowledge of common lymphedema and cancer experiences was also integrated. All video participants were invited to comment on the first edited draft of the video, and their comments informed the final version of the video. Participants also generated the video’s title. The video was then completed and published to the Living with Lymphedema YouTube.com channel.
Methods
In healthcare, the writings of Arthur Frank and Rita Charon have sought to humanize medicine by illuminating the lived experiences of ill people.21-24 These counter-narratives are intended to expand the “narrative resources” available to clinicians during consultations with patients.21 Such approaches are critical with illnesses such as secondary lymphedema after cancer where patient perspectives are under-researched. Our approach to creating the video provided an opportunity for study participants to share their experiences of lymphedema using their own words as well as collages they had created during the aforementioned workshops. Creative writing prompts also helped participants tell their stories during the workshops; this writing also informed the creation of the video.
One of the authors (Gen Allen) of this article was a participant in the Learning to Live With Lymphedema: ‘A New Me’ video. She described her own experiences to the article’s first author, Roanne Thomas, via oral and written dialogues, including e-mail correspondence. Excerpts from this exchange are included below in italics to provide a sample of an individual’s experience with lymphedema through her own words.
Results
The Importance of a Participatory Approach
“We were listened to. We were cared for.”
In this video clip, Thomas explains the participatory nature of the workshops:
Video clip: Roanne Thomas discusses participatory research (3.18 – 3.50)
The workshops and the production of the video were designed to give the participants some sense of ownership and control over content and facilitation. Similar to participatory research, the facilitators’ democratic communication style helped to establish a culture of mutual learning in which the participants’ insider knowledge and contributions were recognized and valued.20,25,26 Allen explains how this shaped her experience:
I believe each of us had control to discuss our story, our struggles, our vision and to express ourselves during each session and through writing or collage. Everyone was given time to express themselves and share with the group through discussions and through their stories or collage projects. Sharing brought more knowledge, comfort and support. It was so powerful. I would say the stories we shared needed to be told and shared – they helped us personally heal & move forward.
The three figures below (photographs of participants’ collages from Study 2) support Allen’s assertions as the images illustrate the range of approaches participants used to illustrate their stories:

Figure 1: A collage with a variety of magazine images of people and travel on a red background. The words “You can be beautiful” were added in handwriting.
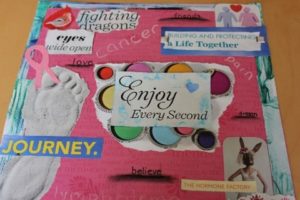
Figure 2: A collage with a variety of magazine images such as a footprint, a bird, and phrases such as “Enjoy every second” and “Eyes wide open.”

Figure 3: A three-dimensional collage designed as a basket on a green and blue background. Paper cranes adorn the basket as well as images such as Northern lights and a bullseye and phrases such as “peace of mind,” “see and feel.”
In addition to the individualized experience, making the collages together provided participants with the chance to interact with others who had the same diagnosis. This was particularly powerful, as Allen explains:
We felt comfort in having similar issues and gained knowledge in sharing stories and coping techniques. Lymphedema needs to be managed daily and is a chronic condition. It is misunderstood by healthcare professionals and by the general public. Compression stockings were something I thought only old ladies wore. Being understood and supported by everyone was so amazingly comforting…having the [rehabilitation] professionals there confirmed some of the tools and techniques we shared with each other and brought on much needed discussion.
Thus, Allen demonstrates the ways in which the workshops’ participatory approach and collaborative group culture allowed for a mutual sharing of stories and support. Following, Gen explains how the arts activities were themselves conducive to self-reflection, facilitating further opportunities to share personal insight and understanding.
Creative Contributions
“Collage tells a story; then in presenting the collage, the story comes out in a colorful way.”
Arts-based research methods are valued for their ability to capture different forms of knowledge.27 In health research specifically, the arts can be used to convey a more holistic understanding that incorporates multiple layers of experience.28 As Allen’s description of her collage reveals, visual and textual narratives contextualize medical conditions such as lymphedema within a person’s life and life story. This, as Alison Cogan suggests,29 can assist clinicians to better understand their patients’ needs—as Allen’s words and her collage (Figure 4) demonstrate:
I had not done anything “artsy” in years. When I started my collage I thought I would not be able to find anything or it wouldn’t mean much to me. Was I ever wrong. I started cutting pictures and couldn’t stop. I gathered up the cuttings, brought it all home and glued everything together. It came together, created a story and showed me what was important to me and painted my story. I still don’t know how it all came together so fast. Two things spoke to me, RETIRE and COTTAGE. I have since retired but do want to continue working and giving back. Part-time work and different from before. Always giving back. As for the cottage, someone asked me (maybe it was Roanne) what it meant to me. We have always had a cottage but sold it after I got sick. Felt we had to simplify our lives and with lymphedema I could no longer water ski Too hard on the bad arm. Well, it made me see that we could still have a cottage but without the big boat. The cottage has always been a place to gather, share time, food and love. We now share our new cottage with friends, family and our grandchildren.

Figure 4: A collage with a variety of magazine images such as an older woman driving a scooter, a cottage and glasses of wine. The text “country living” and “Timeless” are glued onto the red background.
In the video, Allen explains the green and orange sides of her collage, before describing the relationship connecting the two sides. Thus we see how arts-based research methods can be used to convey reflective and narrative processes by linking past, present and future,27 and, as such, have the potential to be hope-enhancing.
One is the cancer side (green) and the other is after cancer (orange). On the green side, the shock, journey, exploration (research, learning), the pen for writing, shoes for walking and exercise, family matters, sunset views (now have a house that has a sunset view), what you see, discovery, binoculars and laughing – the entire learning experience of the cancer and surviving. On the orange side, follow your desire (lady in the dress), see you there (the old folks in the cars on water – anything is possible), wine (I love wine), beach (Hawaii?), claw tub (country living and I love claw tubs – had one installed in June 2018), gorgeous cottage, frog and squirrel (nature), old funky lady on bike (that is me when I am much older) and timeless. They do tell different stories—before and during cancer on the left and living after cancer on the right—follow your desire. When in crisis, do everything you need to and after, LIVE to the fullest.
The process of creating a collage allowed Allen to reflect back on her cancer experience, but, equally important, to think ahead and entertain a more hopeful future.
In the following section, we asked Allen to consider whether the study’s focus on coping skills and hope was significant, both personally and, more generally, for those facing a diagnosis of lymphedema.
Hope and Coping Strategies
The Living Hopefully With Lymphedema workshops that featured in the Learning to Live With Lymphedema: ‘A New Me’ video were designed to foster hope and develop coping skills. In the following section, Allen explains how hope and coping skills were featured in her collage. She then reflects on the significance of hope and coping skills for learning to live with lymphedema:
Hope and coping strategies do come across in the stories. Writing, research, exercise, discovery, family, vision, travel, nature & dreams. After I saw the collage come together, it assured me I was on the right path and had the support of many to guide me further through this journey. The images and story that were pulled together in such a short time were so very powerful. I also enjoyed sharing it with the group as they shared their collages or stories. Very powerful medicine. Natural.
Hope and coping would be my two key themes. When you are faced with such a life-altering change, you need hope. In order to pull you from FEAR to HOPE, you need coping strategies. With a cancer diagnosis, you fear death. You need coping strategies to live again. When you find you also have lymphedema, a life-altering condition you know nothing about and the doctors are not helping, you need coping strategies to give you hope that life will be some kind of normal again.
These ideas and benefits were expressed by all of the participants in the video project. Ryan Hamilton, co-principal investigator in our lymphedema research program, highlights the process of renegotiating “the things that we hope for” that is so evident in Allen’s narrative above. Deirdre Foucauld, another video participant, then explains how she drew hope from the video creation process itself and the understanding that their collective knowledge about living with lymphedema will be passed on to others.
Video clip: Ryan Hamilton followed by Deirdre Foucauld discussing hope (8.08-8.49)
The Role of Narrative and Dialogue
Arts-based methods have been shown to promote dialogue that is highly engaged. For this reason, the arts are used increasingly in research forums as a means to promote reflection, raise awareness and mobilize social action.27,30 Such research is indicative that dialogue can be used to strengthen participants’ collective voice and potential influence in the field of lymphedema education. During the Living Hopefully With Lymphedema workshops, the facilitators actively encouraged the participants to contribute and interact with one another, as this enabled participants to learn from each other while sharing insider knowledge about living with lymphedema. The video co-creation process provided an opportunity for the participants to revisit these conversations and gave rise to “shared meaning” informed by collaborative rather than individual reflection.31
Dialogue is also an important part of educating others in order to improve care as well as to promote hope. For example, Allen offers some very precise recommendations to healthcare professionals about arm measurements and exercise routines in the video.
Video clip: Gen Allen on lymphedema education (7.12-7.42)
Such recommendations come as part of Allen’s new role as a teacher or “expert.” She reflected:
When I look back at the video and see the recommendation, I am very proud. I am also grateful to have been given the opportunity to be heard. My mission is simple and clear. Physio and lymphedema awareness has to be part of the “cancer standard”… An example of changes this awareness has led to is offering help to others through my G.P. When a patient is diagnosed, I am a point of contact for my G.P. if the patient wants to talk to someone. I have helped several people through their cancer and informed them about lymphedema. One lady was in such shock. She was brave throughout her cancer but was struggling so much with her arm as she was an avid skier and was struggling with the first signs of lymphedema. After several phone conversations, we met two times. I coached her and she is now doing very well. I would like to do more!!
Here Allen describes how she has been able to draw from the knowledge and her own experience gained during the Living Hopefully With Lymphedema workshops as well as the video co-creation process in order to support others coping with the same diagnosis. Her testimony powerfully indicates the need for education in the field for both patients and healthcare providers. In the final section of this paper, we reflect on video’s role in meeting this need.
Sharing the Video With an Outside Audience
Upon completion of the video, we invited people living with lymphedema, caregivers, and healthcare professionals to watch the video and share their thoughts. The feedback provided by this audience expressed an appreciation for the clarity of the video, its emotional impact, the diversity of participant experiences, and its educational value for all audience members. One of the video participants suggested it should be “mandatory viewing for all relevant medical professionals such as family doctors, oncologists, radiologists.” Other audience members suggested that the video be shown during cancer information sessions provided by hospitals and cancer centers as well as at conferences for health professionals. In her post-video reflections, Allen elaborates on these suggestions with some very precise recommendations:
I remember someone suggested showing the video to patients at the hospital. You hear about all of the side effects of all of the drugs and family members can attend this information session, but there is nothing about lymphedema discussed. I was given a binder. (I don’t know if they still have that.) I also received a relaxation tape and exercises; the video could be a part of that package. One thought I want to stress is that the video should be shown when families and patients have the info session at the hospital for potential chemo and radiation side effects. Another thought is that the video could be given when the cancer info package is provided to the patient. I was given a CD/tape prior to surgery which had a relaxation tape on one side and walked you through surgery on the other side. My husband and I still listen to the relaxation tape every night (13 years later). Why not put our video on a CD and provide it to the cancer patients as part of the package prior to surgery (if they still get a package)?
Sharing the video at a public screening thus represented an opportunity to foster additional dialogue about the challenges of living with lymphedema and for this community to identify possible next steps. As a result of this event and some additional advocacy by audience members, a lymphedema support group was formed in the city of Ottawa, Canada.
Conclusion
Health professionals may not always have opportunities to examine current literature in fast-paced and demanding working environments. In addition, scientific publications are not always accessible to the general public, both with respect to obtaining the publication itself and to the language used. A video has the advantage of presenting information about secondary lymphedema after cancer by using everyday language supported by images and sound. This medium ensures information is as accessible to patients as it is to healthcare professionals. As an additional benefit, the multimodality of video as a storytelling medium makes these stories and information about lymphedema accessible to people with visual impairments through sound and to people with low literacy skills.
In addition to providing information and support to patients and their caregivers, the Learning to Live With Lymphedema: A New Me video was intended for use in knowledge translation interventions for health professionals, thereby adding value to the research. As such, it was recently incorporated into a free toolkit available online.
The toolkit also contains various components of the intervention (eg, slides, activities) delivered in Study 2 along with guidelines for the creative components. Dissemination through web-based platforms such as YouTube and Facebook make video accessible not only to health professionals but equally, as Allen has suggested, to people living with lymphedema who want to raise awareness of their experiences with family members and friends. The online presence of this video also makes it potentially accessible to audiences worldwide: professionals, those affected by lymphedema or other chronic diseases, and healthcare students, as well as the general public. We echo the participants’ hope that it will encourage dialogue between health professionals and patients, as well as further exploration of psychosocial well-being and its intersections with the humanities—subjects that have received little attention in traditional academic literature.
References
- Brayton KM, Hirsch AT, Patricia J, Cheville A, Karaca-Mandic P, Rockson SG. Lymphedema prevalence and treatment benefits in cancer: Impact of a therapeutic intervention on health outcomes and costs. PLoS One. 2014;9(12):e114597.
- Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N York Acad Sci. 2008;1131(1):147-154.
- Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International Consensus. London: MEP Ltd.; 2006.
- Fu MR, Kang Y. Psychosocial impact of living with cancer-related lymphedema. Semin Oncol Nurs. 2013;29(1):50-60.
- Towers A, Carnevale FA, Baker ME. The psychosocial effects of cancer-related lymphedema. J Palliat Care. 2008;24(3):134-43.
- Deng J, Ridner SH, Murphy BA. Lymphedema in patients with head and neck cancer. Oncol Nurs Forum. 2011;38(1):E1-E10.
- Fu MR, Ridner SH, Hu SH, Stewart BR, Cormier JN, Armer JM. Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology. 2013;22(7):1466-1484.
- Butt CM. Hope in adults with cancer: state of the science. Oncol Nurs Forum. 2011;38(5):E341–E350.
- Duggleby W, Wright K. Elderly palliative care cancer patients’ descriptions of hope-fostering strategies. Int J Palliat Nurs. 2004;10(7):352-359.
- Duggleby W, Ghosh S, Cooper D, Dwernychuk L. Hope in newly diagnosed cancer patients. J Pain Symptom Manage. 2013;46(5):661-670.
- Benzein EG, Berg AC. The level of and relation between hope, hopelessness and fatigue in patients and family members in palliative care. Palliat Med. 2005;19(3):234-240.
- Herth K. Hope in older adults in community and institutional settings. Issues Ment Health Nurs. 1993;14(2):139-156.
- Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Ann R Psychol. 1993;44(1):1-22.
- Heppner PP, Tierney CG, Wang YW, Armer JM, Whitlow NM, Reynolds A. Breast cancer survivors coping with lymphedema: what all counselors need to know. J Couns Dev. 2009;87(3):327-338.
- Krouse HJ. Video modelling to educate patients. J Adv Nurs. 2001;33(6):748-757.
- Duggleby W, Degner L, Williams A, Wright K, Cooper D, Popkin D, et al. Living with hope: Initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage. 2007;33(3):247-257.
- Thomas R, Hamilton R. Illustrating the (in) visible: understanding the impact of loss in adults living with secondary lymphedema after cancer. Int J Qual Stud Health Well-being. 2014;9(1):24354.
- Thomas R, Hamilton R. Composing hope through collage: a community-based intervention for cancer survivors living with lymphedema. Health Psychol Open. 2016;3(2):1-10.
- Hamilton R, Thomas, R. Renegotiating hope while living with lymphoedema after cancer: a qualitative study. Eur J Cancer Care. 2016;25(5), 822-831. doi:10.1111/ecc.12382.
- Hamilton R, Thomas R, Anisimowicz Y, Piers M, Matte, R. A critical analysis of the delivery of a psychosocial workshop for cancer survivors with lymphedema. Qual Rep. 2018;23(10):2586-2602. Available at: https://nsuworks.nova.edu/tqr/vol23/iss10/20
- Frank AW. Just listening: narrative and deep illness. Fam Syst Health. 1998;16(3):197-212.
- Frank AW. Practicing dialogical narrative analysis. In: Holstein JA, Gubrium F, eds. Varieties of Narrative Analysis. Thousand Oaks: Sage Publications; 2015: 33-52.
- Charon R. Narrative medicine: honouring the stories of illness. New York: Oxford University Press; 2016.
- Charon, R. Embodied narrative: living out our lives. J Human Rehabil. 2015. https://www.jhrehab.org/2015/02/01/embodied-narrative-living-out-our-lives/
- Aldridge J. Participation, ‘vulnerability’ and voice. In: Aldridge J, ed. Participatory research: Working With Vulnerable Groups in Research and Practice. University Press Scholarship; 2015:8-30. doi: 10.1332/policypress/9781447305644.001.0001
- Chevalier JM, Buckles D. Participatory Action Research: Theory and Methods for Engaged Inquiry. New York: Routledge; 2013.
- Leavy P. Method Meets Art. Arts-Based Research Practice. New York: The Guildford Press; 2009.
- Weber S. Visual images in research. In: Knowles JG, Cole AL, eds. Handbook of the Arts in Qualitative Research: Perspectives, Methodologies, Examples, and Issues. Thousand Oaks: Sage Publications; 2012: 42-54. doi: 10.4135/9781452226545
- Cogan, A. From surviving to flourishing: using narrative as a tool for patient-centered care. J Human Rehabil. 2016. https://www.jhrehab.org/2016/11/30/from-surviving-to-flourishing-using-narrative-as-a-tool-for-patient-centered-care/
- Riessman KC. Narrative Methods for the Human Sciences. California: Sage Publications; 2008.
- Greenfield BH. Perspective: lessons learned on teaching narrative. J Human Rehabil. 2015. https://www.jhrehab.org/2015/02/01/teaching-narrative/.


 The Art of Happiness: A Handbook for Living by The Dalai Lama and Howard C. Cutler
The Art of Happiness: A Handbook for Living by The Dalai Lama and Howard C. Cutler The Social Dilemma. Netflix Documentary
The Social Dilemma. Netflix Documentary
 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT