INTRODUCTION
This article aims to contribute to a growing body of critical scholarship that illuminates how the field of rehabilitation is structured according to whiteness, in order to drive divestment from this oppressive structure.1-3 We offer this analysis based on the “counter-stories” of nine racialized physical therapy (PT) students and three recent PT graduates regarding their experiences of racism within PT programs in Canada. We recognize that the insights discussed in this paper may be self-evident to some racialized readers. Our aim is not to suggest that we have discovered such experiences within PT, but to offer an analysis of how whiteness infuses the profession—a perspective that is currently absent from the literature.
We are a research team composed of six members who were senior physiotherapy students at the time of the study, five who identify as racialized and one who identifies as white; and two physiotherapy faculty members, one who is a Black clinician educator (MS), and one who is a white critical researcher (SN). We write this article to a PT audience within and beyond Canada, which we understand to be largely composed of people who are white. We begin by introducing foundational concepts related to race, racism and racialization. We then review literature on racism in the context of health professions education in order to set up the need for this study within PT. Our results section illustrates how racism has played out for these students, their responses to these experiences, and how these phenomena are structured by whiteness. We finish by discussing the implications of these findings for taking action in the PT profession to recognize and divest from whiteness. We also reflect on lessons about conducting anti-racism research that we learned through the peer-review process of this manuscript.
Race, Racism and Racialization
Race, racialization and racism structure institutions in North American society,4 including healthcare fields like physical therapy and their clinical training programs. Race is a social construct, without biological basis, that was created historically to justify the subordination of people defined as non-white in order to advance social and economic interests of people defined as white (e.g. enslavement and colonization).5-6 At the center is white supremacy, which Ansley7(p1024) defines as:
“a political, economic and cultural system in which whites overwhelmingly control power and material resources, conscious and unconscious ideas of white superiority and entitlement are widespread, and relations of white dominance and non-white subordination are daily reenacted across a broad array of institutions and social settings”
The field of critical race theory (CRT) investigates and illuminates how white supremacy and its subordination of racialized people has become entrenched and normalized throughout societal institutions, including education and healthcare.8-11 CRT challenges ahistoricism and requires linkage of present-day racial inequities with historical antecedents. CRT recognizes the experiential knowledge of racialized people as legitimate and crucial for understanding racial subordination. CRT is both intersectional and interdisciplinary in its approach to understanding and transcending the complexities of racism and oppression.12 Importantly, CRT is a form of social justice praxis in its commitment to “link theory with practice, scholarship with teaching, and the academy with the community.”13 The goal is not just to illuminate racial injustice but to change it.9
One way that racism is reproduced is through perpetuation of the idea that racism is individualistic (i.e., the intentional behavior of hateful people) and not societal (i.e., institutionalization of a system of inequality).4 As such, claims of racism toward people defined as white are frequently met with outrage or denial since white individuals believe they have not behaved in intentionally hateful ways.14 Interrupting this misunderstanding and coming to see racism as a structure and not an event is crucial for addressing disparities and harms.15 However, the social structure of racism also sets the context for harmful interpersonal interactions based on prejudice and stereotypes.16
In this paper, we conceptualize racism according to Jones’ three-level framework: institutional, personally-mediated, and internalized racism.16 The first level, institutionalized racism, reflects the structural factors in society that produce disparities between white and racialized groups, such as unequal access to services and opportunities. Personally-mediated racism reflects person-to-person incidents of prejudice and discrimination based on race. Jones’ third level of racism, internalized racism, is defined as an individual’s self-acceptance of the perceptions that society places on her/his abilities and intrinsic worth leading, for example, to individuals within a racialized group devaluing themselves or others of the same race. Jones’ framework has previously been used to explore experiences of racism among racialized PTs and Indigenous medical students in Canada, and as a framework for conceptualizing racism in health research.17-19
Research on Racism in the Context of Health Professions Education
Research on racism in healthcare education programs has focused largely on perceptions about race and the experiences of racialized students. Roberts et al explored students’ perceptions of race at two British medical schools, finding four themes: “white fears” when discussing race-related issues, discomfort with being viewed as “different,” inability to relate, and barriers against talking about race.20 Sedgwick et al investigated the experience of racialized nursing students, noting that their sense of belonging was enhanced or diminished by their interactions with nurse educators.21 In the Canadian context, Beagan found that third-year students at a Canadian medical school who are racialized experience daily practices of racism, and that dealing with these harms is an added challenge to their education.22 Martin and Kipling found that the experiences of Indigenous students at two Canadian nursing schools were shaped, in part, by racism from individuals, groups, and institutions.23 In 2017, Anderson DeCoteau et al reported far-reaching experiences of institutional, personally-mediated and internalized racism among medical students at a Canadian medical school.18
There is no published research investigating experiences of racism among physiotherapy students in Canada. However, Hammond et al reported three themes derived from focus groups with 17 racialized PT students in South East United Kingdom: feeling like an outsider in reflections of belonging, behaviors by others that marginalize, and personal strategies to integrate into PT despite lack of power and influence.24 Further, there is a small body of research exploring racism in physiotherapy practice more broadly. Studies by Yeowell25 and by Vazir17 et al both reported on the dominance of white culture within physiotherapy, which can lead racialized physiotherapists to feel out of place. In a survey of 420 British PTs, Bogg et al found that two-thirds perceived that racialized PTs were underrepresented in the profession.26 Haskins et al investigated the role of covert bias in the evaluation of physical therapy students by asking clinical instructors to assess a white, Hispanic, Asian, and Black student, each of whom used the same script to report on a patient; the Black student was consistently given lower ratings despite reciting the same script in the study videos as their counterparts.27 Norris et al retrospectively analyzed assessment marks from 1851 PT students at four institutions in South East United Kingdom, finding that non-white students were awarded significantly lower scores than their white counterparts.28
Missing from these studies is explicit engagement with critical race theory and problematization of the white supremacist underpinnings of these fields that give rise to these harmful experiences. However, critical race scholarship is beginning to emerge in the rehabilitation sciences. First, James et al identify how the field of rehabilitation science “absents” the role and impact of race and racialization, thus reproducing structural racism.1 Grenier draws on critical race theory to illuminate how anti-Blackness, anti-Indigenous colonial relations, and Orientalism have and continue to influence how occupational therapy is taught and practiced in Canada.2 Further, Omar et al are using critical race theory to inform a scoping review of rehabilitation among Black people with traumatic brain injury.3 Our study builds on these bodies of research by exploring counter-stories among racialized students in Canadian physical therapy programs regarding experiences of racism and how they manage these experiences.
METHODS
Study Design and Participants
This study draws on critical race methodology in that it foregrounds the structuring role of racialization throughout the research project and seeks to disrupt taken-for-granted assumptions about race through the counter-stories of people who are racialized.29-30 This approach recognizes the experiential knowledge of racialized people as critical to understanding racial subordination. The counter-story, a method of telling the stories of those whose experiences are not often told, is a tool for exposing, analyzing, and challenging the dominant stories that reproduce racial privilege.29 In order to hear counter-stories about experiences within PT education, we recruited English-speaking participants who (1) self-identify as racialized, and (2) are currently enrolled in and have completed at least four months of a MScPT program in Canada, or graduated from a Canadian MScPT program within the last two years. We excluded current University of Toronto MScPT students due to concerns of power differentials and potential sensitivities with faculty co-advisors and student researchers. We also excluded internationally-trained physiotherapists in a bridging program in Canada.
In addition to these criteria, we purposively sampled for racial and geographical diversity among participants. Specifically, we aimed to recruit at least two Black and two Indigenous participants in order to invite counter-stories related to anti-Black and anti-Indigenous racism in particular. We also sought to recruit at least two participants each from MScPT programs in the following geographic regions in Canada: Western (University of British Columbia, University of Alberta, University of Saskatchewan, University of Manitoba), Central (Western University, McMaster University, University of Toronto, Queen’s University, Université d’Ottawa), and Eastern (McGill University, Université de Montréal, Université de Sherbrooke, Université Laval, Université du Québec à Chicoutimi, Dalhousie University).
We used a combination of purposive and snowball sampling to recruit participants.31 Recruitment e-blasts were sent to members of the Canadian Physiotherapy Association’s Global Health Division. Additionally, emails were sent to PT contacts across Canada who were known to the research team to disseminate the recruitment letter and refer potential participants for the study. Interested participants contacted the study team and scheduled an interview time. A follow-up recruitment email was sent through our professional networks approximately three weeks later, and a final call for recruitment was sent again two weeks later seeking the outstanding racialized and geographic groups for our sampling targets.
Data Collection
We developed an interview guide based on the objectives of our study and Jones’ levels of racism.16 The interview guide comprised: (1) open-ended questions inviting stories about how race influenced the participant’s experience as a PT student, (2) open-ended questions exploring how the participant responded to or managed their experiences with racism within the PT program, and (3) open-ended questions about the participant’s perceptions of racism in the PT program in general. The interview guide was pilot-tested with three current University of Toronto PT students who identified as racialized but did not fulfill the recruitment criteria. In-depth, one-on-one, semi-structured interviews, each lasting 30-60 minutes, were conducted in private rooms by phone or Skype according to the participant’s preference. Interviews were conducted by three team members, each of whom was an MScPT student who identified as racialized. All interviews were audio recorded. Following the interviews, the audio recordings were transcribed verbatim by a research team member who did not conduct the interview and then quality checked by the original interviewer.
Data Analysis
We followed Flicker and Nixon’s six-step DEPICT model for collaborative qualitative data analysis.32 First, each transcript was read by at least two researchers to identify patterns of ideas in the data. We then collaboratively used these ideas to inductively develop a draft coding framework, which we pilot-tested on half of the transcripts and then finalized. The final coding framework was used to code each transcript, and we used NVivo (Version 11.4.1), a qualitative analysis software, to help us organize the coded data. We assigned subgroups of our research team to develop summaries of the data in each coding category, which we shared in writing and verbally at a series of analysis meetings. During these meetings, we reflected on how participants’ stories helped address our research questions. We also reflected on how Jones’s framework helped make sense of the findings. During the manuscript revision process, we welcomed the recommendation of a blinded reviewer to engage more directly with critical race theory in both setting up the article and making sense of the results. In this way, we developed an analysis based on the counter-stories of participants that was mediated by the scholarship of Jones and other critical race theorists.
To maintain confidentiality, participants are identified numerically (e.g., Participant 1, Participant 2). This study was approved by the Health Sciences Research Ethics Board at the University of Toronto.
RESULTS
Nine current PT students and three recent PT graduates were interviewed (see Table 1). These 12 participants were from 9 different MScPT programs across central and western Canada. Participants included 9 females and 3 males. Three participants identified as Black, 2 as Asian, 5 as Chinese, one as Middle Eastern, and one as Latin American.
Whiteness Shapes the Experiences of Racialized PTs
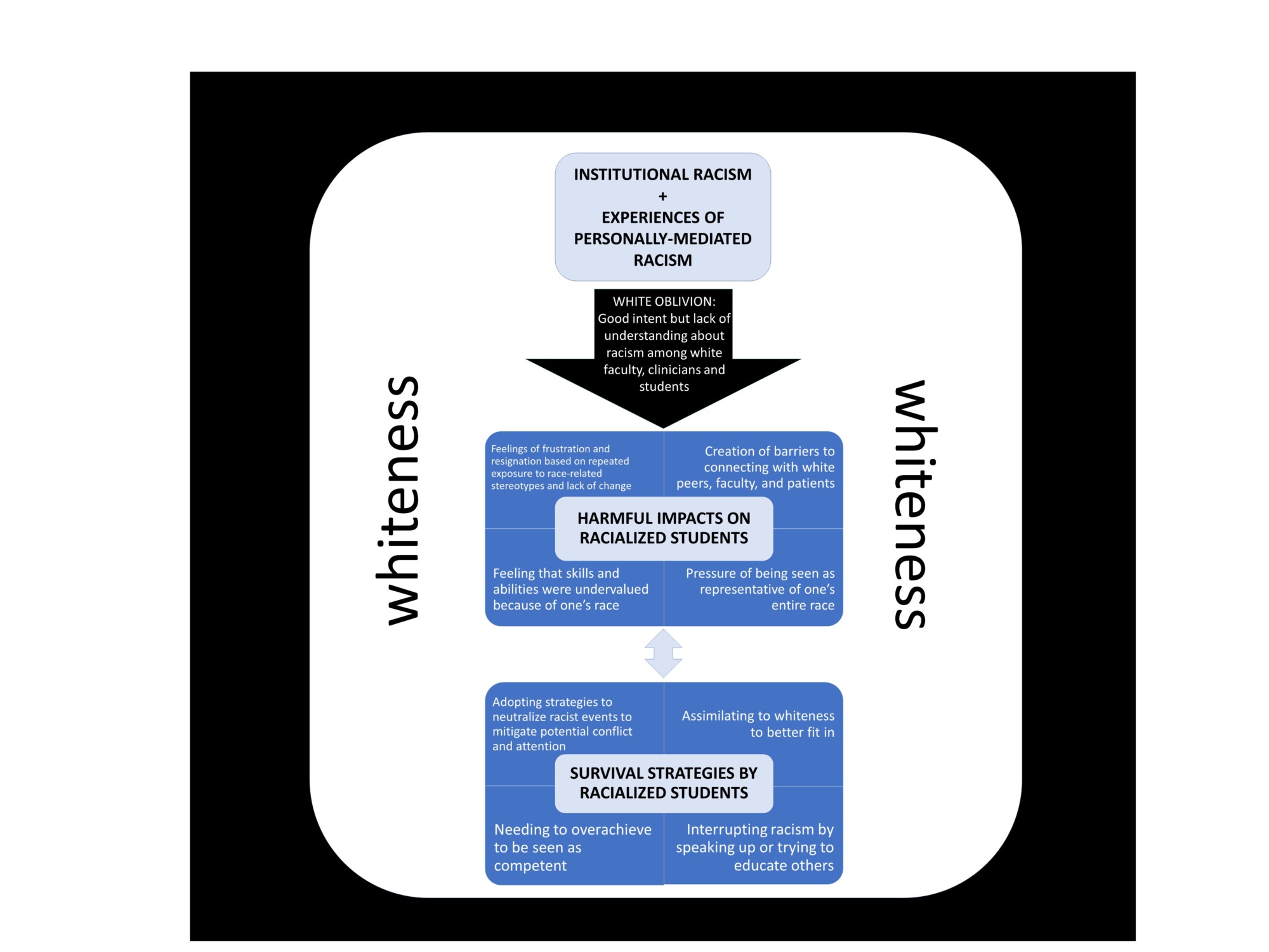
Participants were asked to reflect on how race and racism influenced their experience as PT students. Their counter-stories described institutional and personally-mediated forms of racism experienced against the backdrop of a culture of whiteness. They explained how these forms of racism were upheld by white oblivion, whereby white faculty, students and patients had good intentions but lacked understanding about structural racism and their complicity as part of this system of inequality. Participants also described how they were impacted by these experiences, and how they responded to cope with or mitigate the harms of these situations (see Figure 1). Below we present these findings in detail.
Institutional and Experiences of Personally-Mediated Racism
Institutional racism was described as central to participants’ experiences of racism and linked with their related impacts and responses. Participants often referred to the lack of racial diversity in PT, describing PT as a white profession, especially when considering leadership roles. Furthermore, participants noted that some white faculty members or clinical instructors appeared to show less understanding and empathy toward racialized students, resulting in an inequality of access to learn or practice skills even when participants voiced different learning needs. This example exemplifies the interlinkage of personally-mediated and institutional racism, as described by Jones.16 For example, while an institution added a screen in clinical labs to respect a participant’s cultural boundaries regarding undressing, she explains how it failed to create an equal learning environment:
“I thought that was a good suggestion and we went ahead and got the screens. When it came time to use them in class, nobody really wanted to go behind the screen because it would be difficult to see what others were doing if you wanted to ask a question. So it wasn’t very successful. It particularly wasn’t successful when a professor asked me not to use the screens. A professor said, ‘I don’t want you taking a [teaching assistant] back there and then that particular section of the class wouldn’t have a [teaching assistant].’ In my mind I thought, you know, it’s no different than a teaching assistant standing at a plinth and speaking to two students. I’m not sure why the screen makes it any different. But again, as a student, I had no choice but to go with, um, what the professor had suggested.” (Participant 8).
Participants often reported feeling that they had no one to advocate for them when facing discrimination based on their race. Further, they described a lack of safe avenues for support through the PT program or placement site regarding concerns about racism. One participant described how the school responded when dealing with a preceptor who the participant felt was giving them a negative evaluation due to race: “[I] explained to the school my situation and they didn’t really empathize at all” (Participant 5). Another student explained how they had to respond to incidents of racism from patients on their own: “I feel like a lot of the time the clinical instructor wouldn’t be the one to intervene; I would actually need to speak up for myself.” (Participant 10).
Personally-mediated racism was identified by participants through interactions with patients, classmates, teaching faculty and clinical instructors. Examples included undervaluing participants’ skills and abilities, repeating common racial stereotypes, and negatively evaluating the individual’s clinical competency based on perceptions associated with their race. Participants also described feeling excluded by white classmates in clinical labs, by patients not wanting to receive care from them because of their race, and by clinical lab assistants spending less time with racialized students. One participant shared this experience of personally-mediated racism in a patient interaction:
“He [the patient] continued to speak in derogatory terms about me and about other staff members who were also colored, and then I had to chart it. So as I charted it, it was quite emotional because I had to write word for word all the swear words and derogatory comments that he had said about me” (Participant 8).
White Oblivion: Good Intent, But Lack of Understanding About Racism Among White Faculty, Clinicians and Students
In addition to the act or event itself, participants emphasized that benevolence and/or oblivion regarding racism shaped the impacts of and their responses to racism. For instance, in response to an unsettling racist incident with a patient, Participant 1 was told by their instructor: “I hope you didn’t think that was offensive; it was just him being playful.”
The intent of the perpetrator was rarely presumed to be negative, despite the harmful impact. Furthermore, participants regularly reflected on the lack of understanding about racism among white peers and faculty. For instance, Participant 4 explained,
“[My peers] will say things, and I know they are not saying it because they’re trying to be rude, but they are saying it because they just don’t know.”
Harmful Impacts on Racialized Students
The impact of participants’ experiences of everyday racism was seldom described as the result of a single event. Rather, participants shared 4 types of responses shaped by single and collective experiences of racism. Overall, these impacts produced a burden carried by these racialized students that was deemed likely to be invisible to white faculty.
- Feelings of frustration and resignation based on repeated exposure to race-related stereotypes and lack of change
Some participants reported a sense of futility or feeling as though there was nothing they could do to change their experiences of racism. They explained that it was something they have always had to deal with and will have to deal with in the future. One participant expressed frustration because, “A lot of people will assert that racism doesn’t exist in Canada, which is not true.” (Participant 3). For example, participants commonly voiced frustration with having to explain their ethnocultural background to white patients, which is a common microaggression based on the idea of whiteness as the default norm in Canada. When subjected to these or other racial stereotypes, participants expressed feeling frustrated when white individuals were unable to understand why their words may have been offensive.
- Creation of barriers to connecting with white peers, faculty and patients
Participants explained how answering inquiries about their race heightened their sense of “not belonging” in the PT profession. Further, they explained how responses of defensiveness, denial or dismissiveness around issues of race created barriers to connecting with patients, peers and faculty. For instance, one participant stated, “Patients would often ask me things like, ‘Oh, are you Japanese? Are you Korean?’ And I say, ‘No, I’m actually Chinese and I identify as Canadian.’ Then they would say, ‘Well that’s not what I was asking! I was asking where you are from.’” (Participant 9).
Other participants reported that the lack of racial diversity among faculty, and concerns about the inability or unwillingness of white faculty members to engage meaningfully on issues of racism, exacerbated difficulties they experienced in the program. Participant 3 explained: “Leadership roles who were predominantly white women; I felt like I could not really open up to them.”
- Pressure of being seen as representative of one’s entire race
Participants reported that there were few other students of their racialized identity in the program. As a result, participants felt that assumptions would be made about their entire race based on their behavior as an individual. They described pressure to exemplify their race positively to avoid reinforcing negative stereotypes. Participant 1 described this feeling:
“I know that I just feel that everyone sees [my race] first, so I’m very careful, very, very careful, with how I present myself. …I always try to carry myself differently because…if this person is going to form an opinion of Black people, cause I’m the only Black person they know, that they are going to form an opinion of the whole race. I better be good. I better show up on time. I better do this. It’s a lot of pressure.”
- Feeling that skills and abilities were undervalued because of one’s race
Many participants described needing to work harder to be seen as competent relative to their white counterparts. As one participant explained, “It was like this sort of pressure in a way to already be better or to be a good student so you can be on the same level as everyone else.” (Participant 12). The same participant explained the toll of this enduring pattern:
“Race and ethnicity are always, always in the back of my head because there are not a lot of people in my, in our profession that are from my background. So that always makes you wonder a little bit, you know? Is he going to like me, or does he like my classmate better because of this or because of that, or is this actually a race thing that is involved? I don’t think I ever truly got an answer to those questions, but those are questions that always popped up in my head when I would start a new clinical placement.” (Participant 12).
Survival Strategies by Racialized Students
Participants described 4 types of responses employed to manage, mitigate and survive their experiences of racism.
1. Adopting strategies to neutralize racist events to mitigate conflict and reduce attention
In response to incidents of racism, participants commonly described responses designed to neutralize the situation. For instance, participants often “laughed it off’ as a way to absorb the harm and end the incident. Most participants described these racist events as stemming from the perpetrator’s ignorance rather than malicious intent, but wished others understood the impact of these actions. As one participant stated:
“I’d like them to understand what is actually going on in the situation, but I don’t want to make it a big thing and then make people feel uncomfortable, even though I wish they were…more educated on the matter.” (Participant 11).
- Assimilating to whiteness to better fit in
Some participants described changing the way they spoke to patients to assimilate to white culture in order to better connect with patients. One participant described how they change their voice when working with white adults:
“I don’t know if you see how Black comedians tend to, when they’re impersonating white people, they perk up and make their voices sound a certain way. I do that to a lesser extent but not quite as exaggerated, but there’s definitely that change in tone and word choice.” (Participant 11).
Some participants identified the concept of being “white-washed” to describe racialized individuals, including themselves, behaving in a way that is aligned with white culture to try to fit in.
- Needing to overachieve to be seen as competent
Participants often responded to the pressure they felt by working harder to be seen as competent and to counteract the risk of their skills and achievements being judged based on racial biases. Participant 6 described this pressure when relaying their experiences in the classroom setting:
“I’ve taken that approach of just always making sure that I’m on the ball, always making sure that my knowledge base is a little bit higher…because it will create difficulties if I haven’t prepared for a particular project, or a presentation very well. It kind of gives people an opportunity to basically discredit my work and be dismissive in the future.”
Participants explained that they had to adapt and develop “soft skills” to manage experiences of racism and be recognized for their achievements. Participants described having improved communication skills, greater tolerance and understanding of the differences of others, and stronger work ethic.
- Interrupting racism by speaking up or trying to educate others
Several participants took the approach of interrupting racist encounters by trying to educate others on race and racism, either through direct conversation with individuals or through creating a dialogue on their social media platforms. Participant 8 explained:
“My social media is just very open and positive and inviting to questions…I always try and keep that openness there so if they do have a question, and even maybe 2 years down the line, somebody may come around and ask me a question, then it’s there. I think that’s just how our culture is with being open, and with being receptive to answering people’s questions and being a good role model as a human being.”
DISCUSSION
Advancing Understanding of Racism in the Context of Health Professions Education
This is the first study to explore perspectives of racism among racialized students in PT programs across Canada. Our findings with PT students paralleled the findings by Vazir et al with racialized PT clinicians in Canada regarding experiences of institutional and personally-mediated racism in the context of the everyday PT roles.17 Our results also align with the experiences of marginalization reported by racialized PTs in the UK.24 Further, our participants’ narratives also echo literature investigating experiences of racism among racialized students within nursing and medical programs regarding lack of non-white faculty role models, a feeling of not belonging, lack of understanding and acknowledgement of racism from faculty and peers, and segregation (or an “invisible barrier”) from the dominant group.20-22 We add to this literature by also identifying strategies PT students use to survive these experiences of racism within their program, including neutralizing racial events, assimilating to dominant culture of whiteness, working harder to be seen as equal, and confronting racism by educating others. Some of these strategies aligned with a study investigating approaches for managing racism and homophobia among racialized gay men in the United States, including dismissing the stigmatization, direct confrontation, dissociating from social settings, and drawing strength from external sources.28
We also add to previous literature, particularly within PT, by engaging critical race theory to inform the analysis. This theoretical orientation frames race and racism as set against the historic and contemporary backdrop of white supremacy, which makes possible conclusions around the need to divest from whiteness as opposed to tinkering within this oppressive system.11 In line with this framing, our results highlighted two processes that uphold racism within the PT education context.
The first is oblivion among white people that racism is a social structure that upholds whiteness as the ideal.34,35 That is, the erroneous belief that racism is exclusively the intentional action of bad people, as opposed to a system of inequality of which we are all part. As racialized poet Guante explains, “Remember: white supremacy is not a shark; it is the water.”36 The finding of white oblivion may be informed by the concept of “white ignorance,” which Jamaican philosopher and critical race scholar, Charles Mills, discusses in part as the ways that white people are unable to understand the world that they have made.37,38
The appeal to ‘color-blindness’, in which white people presume to not see color as an anti-racism strategy, serves to uphold and reinforce racism by dismissing the vastly different social experiences of people who are racialized versus those who are white.39 Our participants described how the structural and institutional nature of racism fostered the environment whereby personally-mediated events could be seen as acceptable, or something to be laughed off. Personally-mediated experiences reported from students were often attributed to the naïvete of white individuals regarding their own racist behaviors and attitudes. In other words, the narratives were largely about good individuals unwittingly upholding racism because of oblivion about their place in this social structure, which raises the issue of intent versus impact. Participants commonly described a discrepancy between what white individuals intended to communicate about a topic involving race and the harmful impact of their words or actions on the racialized students, such as questioning where one is from. Wang et al call this type of incident a “racial microaggression,” ie, conversations that seem innocuous to white individuals but can be harmful to racialized people.40 Others have critiqued this term on the basis that there is nothing “micro” about the harm that is inflicted.41
The implication for the PT profession is to reject the faulty premise that racism is based on intent and is something that only bad people do. Rather, the goal is to understand that racism structures institutions and is something that all people are socialized into by virtue of being part of society. The question is not whether one (and one’s field) upholds racism but how. Making complicity in this system visible gives the power to change actions and re-imagine our profession to reduce these harms.30,42,43
The second process is “white fragility,” or the myriad ways that white people are socialized to respond when asked to consider their complicity within the social structure of racism, such as denial, guilt, outrage and defensiveness, each of which serves to protect the status quo.6,14 Indeed, one might expect such a reaction among white readers of this and other articles that seek to illuminate structural racism and consider divestment from whiteness in the context of health care. In our study, white fragility appeared in narratives about racist events being dismissed or diminished by white faculty or clinical instructors. While this may be a new concept for many people who are white, these characteristic responses are typically well known to those who are racialized.6,35 Anticipation of white fragility frequently shapes how racialized people handle racist events in order to avoid the frustration of this typical response. In our data, this is seen in the narratives related to participants wanting to protect the feelings of white people and minimize their discomfort regarding issues of racism. This work of managing everyday racism, including responses related to white fragility, is a challenge likely faced by many racialized PT students, which is largely invisible to white faculty, clinicians and peers. The opportunity, and indeed imperative, among white PT leaders is to come to see and transcend this fragility in order to meaningfully engage in accountable anti-racist action to work toward ending white supremacy.
Where From Here?
The insights raised in this study regarding some of the ways that the social structure of racism plays out through PT educational programs in Canada may be transferable to PT programs in similar jurisdictions, including the United States, Western Europe, Australia and New Zealand. In particular, our findings have implications for academic institutions in Canada, as well as the policies outlined by the National Physiotherapy Advisory Group. This group represents a coalition of national PT-related organizations in Canada that promotes the provision of quality PT services and positive health outcomes for Canadians.44 In light of the results, universities and clinical sites should commit to understanding and reducing institutional and personally-mediated racism to create more equitable opportunities for success among all students.45 In her recent analysis, Dr. Tracy Blake noted that the near absence of anti-racism resources, training, policy and procedures within physiotherapy education, regulation, and advocacy institutions in Canada has resulted in a Canadian physiotherapy sector that is unprepared to contribute to the disruption and dismantling of racism in healthcare as well as within the profession itself. 46
First is the need for education among faculty and PT leaders regarding anti-racist practice.47 This involves learning about the structure and techniques of racism, the identity of whiteness, and the reorientation required to work in solidarity to dismantle white supremacy.1,42 We note the caution from Boyd et al regarding the current focus on implicit bias training, which they argue “stalls progress to end inequities by entreating clinicians to tame ‘unconscious beliefs,’ rather than confronting explicit practices that undergird systemic inequities.”48 Rather, this work requires deepened understanding of the history of how the institution of healthcare, including rehabilitation, has been a tool for oppressing racialized people, in order to understand the role of physiotherapy education in reproducing present-day inequities.49 Developing insight among those who control the curricula and professional standards sets the stage for embedding transformative anti-racist practice and education throughout PT programs. This includes a focus on anti-Black and anti-Indigenous racism. Related is the need for building capacity regarding cultural safety, which is an approach developed by nurses in Aoterea/New Zealand to respond to the inability of the mainstream healthcare system to meet the needs of Maori People.50 Cultural safety requires change in terms of both personally-mediated forms of oppression, and also the wider systems of power (including racism) that create unsafe environments for Indigenous peoples to seek and receive quality care. Churchill et al identified 7 evidence-based, wise practices for cultural safety education that may be applied to other racialized groups as well, such as creating learning spaces that support non-Indigenous people, to learn from their discomfort.51
Second is the need to create a safe means for students to discuss and report incidents of racism experienced within PT. A community of support for racialized students, which includes and is led by racialized PTs, could contribute to building such a safe space. As such, it is crucial to increase the recruitment and retention of racialized PTs across programs and clinical sites, and particularly among leadership roles in the profession. Furthermore, as many of the experiences involving racism occurred during clinical internships, universities and clinical sites should provide students, clinical instructors, and site coordinators with guidance on how to manage such incidents in the moment as well as at the institutional level.
The National Physiotherapy Advisory Group identifies diversity under the essential competency of Professionalism, stating that physiotherapists must “behave in a manner that values diversity.”44 However, valuing diversity is necessary but insufficient for mitigating racism. The profession must be open to re-imagining itself in a way that embraces and centers equity, inclusion, and a sense of belonging among racialized clinicians, educators and students.
Lessons We Learned about Anti-Racist Scholarship During the Revision Process
Health-related research on racism, including in the rehabilitation sciences, has been rightly critiqued for reproducing as opposed to challenging the norms of white supremacy.1,48 An earlier version of this manuscript unwittingly fell into this trap in several ways, which were brought to light by a reviewer with expertise in critical race theory. Given our interest in using rehabilitation research to illuminate and help dismantle white supremacy, we are taking the unusual step of making explicit 3 of the ways that our initial manuscript reproduced the very structure we were trying to destabilize.
- Assuming a white audience. Amir Jaima notes: “There is a discursive tendency when examining questions of race and racism to address a reader who is implicitly white. …In addressing a white reader who is potentially hostile, or suffers from ‘white ignorance,’ we find ourselves beginning our analyses, not from a historiographic survey of the question, but from a pre-emptive justification that we should continue to pose it at all.”38 This tacit assumption of a white readership allows for research on racism to present such experiences to be framed as discovered and novel, as if they are not already well-known to people who are racialized. To address this concern, we made explicit the audience to whom we wrote this article; namely, the profession of PT, which is largely white. We also audited the article for the myriad ways we softened language to avoid triggering white fragility among our potential readership, and elected to revise the manuscript using more straightforward language about racism and white supremacy. Jaima calls for critical race scholars to “explicitly reorient our discursive voice toward a non-white reader,” which helped us realize that we are unaware of any anti-racist rehabilitation scholarship that is intentionally written for a racialized audience —and is thus a crucial direction for future research.38
- Focusing on experiences of racialized people as opposed to the structure of white supremacy producing these experiences. Research on experiences of racism can focus the reader’s gaze on the racialized individuals (i.e., the racialized students in our inquiry), with the goal of interrogating their experiences, while allowing the structure of the institution (ie, the PT profession and PT educational programs in our inquiry) to go unexamined.48,52 Nixon seeks to translate this argument using the Coin Model of Privilege and Critical Allyship, where she notes the focus on the bottom of the coin (i.e., people from groups that are pushed to the margins) as opposed to the coin itself (i.e., the social structure causing inequity).35,43 The focus on racialized students can lead to conclusions about the need for making more room for racialized people in the current environment as opposed to calls for dismantling the white underpinning of the field in line with the white supremacist underpinning of all societal institutions. To address this concern, we revisited our results to more clearly problematize whiteness as the problem we are trying to understand through the insights of our participants —and to remove places where we had unwittingly positioned racialized students as the problem under investigation.
- Failing to center critical race theory and theorists on research related to race. Critical race theorists argue that analysis of racism must be nested in the historic context of racialization, which positions the field of PT no differently from other aspects of racialized students’ social worlds that are also structured by racialization.5 Further, ignoring this vast body of critical scholarship also serves to further marginalize and silence, as opposed to center, the (largely) racialized thinkers who have produced and advanced this thought. To address this concern, we began by reading more deeply on the work of critical race theorists, and exploring how core concepts in CRT aligned with and deepened our analysis. We are continuing to grow in this area.
Limitations and Future Research
This study had a small sample size, indicating that findings open up new insights about this relatively unexplored topic but should not be considered the entire story. Many more voices and perspectives are needed to understand the complexities of how the societal structure of racism is reproduced in PT programs, especially from those not included in this initial inquiry, including Indigenous PT students, and racialized students who are Francophone and/or from programs in Eastern Canada. We note that none of the research team members had formal training in critical race theory, which suggests that there may be further nuances of this inquiry that our team may have overlooked. Furthermore, it was beyond the scope of this study to conduct intersectional analysis, which is a tenet of critical race theory, regarding how gender and other social structures shape experiences of racism.
Operational research is dearly needed to explore how to effectively embed and scaffold education on anti-racist practice and cultural safety throughout MScPT curricula and professional development for faculty. Future research should also investigate racism and anti-racist practice in other rehabilitation programs such as occupational therapy and speech and language pathology, given their similar patient populations, clinical settings, and educational approaches. These studies must focus on mechanisms of racism within PT and rehabilitation more broadly.
CONCLUSION
The study illuminated experiences of racism among racialized students in Canadian PT programs. The impacts of racism, which were underpinned by good intent but lack of understanding, included feelings of resignation, the creation of social barriers, feeling undervalued, and pressure due to feeling seen as representative of their entire race. Participants responded by neutralizing situations, assimilating to the dominant culture to fit in, addressing racism by speaking up or educating others, and overachieving to be seen as competent.
A key finding was the perception of hopelessness among participants that the current state of institutionalized racism among the PT profession was unchanging and must be accepted as the nature of the profession. This hopelessness is a direct call to those in formal and informal leadership roles at all levels of the profession to reflect critically on our collective roles in upholding racism, and to act in solidarity to disrupt this harmful system.



 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT