Neuromuscular Scoliosis (and Resolution) as a Lived Experience for an Adult With Tetraplegia
By Jennifer Hastings PT, PhD, NCS
Abstract
Background: Neuromuscular scoliosis is a common secondary complication following spinal cord injury (SCI). The common assumption in the literature and among medical professionals is that neuromuscular scoliosis is inevitable in individuals with damaged nervous systems who require full-time wheelchair use. Therefore, considering new-onset scoliosis as a treatable condition, not a permanent, inevitable complication, has significant quality-of-life implications.
Objective: The research question that guided this study was: What is the lived experience for an individual with tetraplegia with new-onset neuromuscular scoliosis? More specifically, how did this condition impact his function and quality of life? And, what was the lived experience of interactions with healthcare providers during this episode of care?
Method: Our participant was not specifically selected for this study; rather, he selected the researchers to investigate his lived experience. Our participant was compelled to share both the emotional turmoil of his experience and the successful outcome to provide research that will change the future approach to treating SCI individuals dealing with neuromuscular scoliosis. A phenomenological inquiry was conducted with qualitative comments extracted from our participant’s journal, medical records, and an interview and observations with our participant. Thematic analysis was conducted on all generated text.
Results: The themes identified were: (1) feelings of social isolation, (2) diminishing productivity at work, (3) losing control of function, (4) decreased independence, and (5) negative mental status. Resolution of the scoliosis reversed the downward psychosocial spiral.
Conclusion/Clinical Implication: This study offers a critical description regarding the lived experience of dealing with the psychosocial implications of the development of new-onset neuromuscular scoliosis in an individual with chronic SCI.
KEYWORDS: Scoliosis, Quality of Life, Tetraplegia
Introduction
Approximately 282,000 people in the United States live with spinal cord injury (SCI); an estimated 17,000 new cases occur each year.1 The injury greatly impacts young adults, typically those aged less than 30 years. Some authors report as high as 80 percent of SCIs occur in males.2,3 The extent of the neurologic injury varies depending on the location of the damaged spinal cord. Cervical spine injuries result in tetraplegia (impairment in trunk and all four limbs), whereas thoracic and lumbar spine injuries typically result in paraplegia (some degree of trunk impairment and impairment of lower limbs). Learning to cope with such an injury can be a lifelong process, from the initial shock of the trauma to incorporating newly learned skills for performing daily activities. Paraplegia and tetraplegia not only impact the function of the physical body, but also carry psychosocial implications.
Depression and reports of low body image are common responses to a sudden traumatic SCI in which the individual is forced to redefine themselves and their life roles.4 This life-changing medical event can stimulate deep emotions related to loss of function, disability, and loss of independence. Learning to function physically with paralysis and the social stigma of using a wheelchair are huge challenges that individuals with new tetraplegia encounter during rehabilitation and throughout their lives. After this traumatic event, it takes perseverance to regain a sense of control of one’s life and to function independently. A study that researched the predictors of physical and mental health in adults found that the ability to be independent from others has the greatest positive impact on overall health.4
Co-morbid injuries or serious changes in health status are difficult for anyone to cope with; however, co-morbidities can be exacerbated in individuals with SCI who depend on a wheelchair for mobility because of the mental and physical challenges they already face daily. The development of secondary complications such as neuromuscular scoliosis can be physically debilitating to a person with tetraplegia because it impairs their functional ability to transfer, sit comfortably in their wheelchair, and perform activities of daily living. There is also an immense impact on psychological health because of the negative body image caused by a new spinal deformity. New-onset scoliosis may be particularly stressful for individuals with SCI due to the loss of the independence they worked hard to develop during their initial rehabilitation. However, how individuals experience such conditions has not been described. Thus, the purpose of this study was to uncover the lived experience of a man with tetraplegia and new-onset neuromuscular scoliosis, and the successful resolution of the new condition through nonsurgical interventions.
A Common Secondary Complication
Neuromuscular scoliosis is a common secondary complication following SCI, occurring due to neuromuscular imbalances that can eventually lead to complications including chronic pain, pulmonary insufficiency, and reduced lung capacity.5 The impact of these complications can dramatically limit independent self-care, negatively influence the individual’s quality of life, and be life-threatening.6
Once neuromuscular scoliosis is established in a person with tetraplegia, misalignment of the joints can create a noxious stimulus, which increases spasticity that may contribute to further muscular contracture, establishing a cycle of worsening scoliosis. The common assumption in the literature and among many medical professionals is that neuromuscular scoliosis development is inevitable in individuals with damaged nervous systems who require full-time wheelchair use; a traumatic paralysis of the cervical spine is said to have a 100-percent incidence of developing scoliosis within 10 years of the originating injury.7 The majority of research focuses on surgical correction of neuromuscular scoliosis; there is a significant lack of research into conservative interventions.
Current Treatment Options
Current treatment options to correct neuromuscular scoliosis include spinal bracing and surgical fusion; however, these options present many drawbacks. Although spinal bracing limits the progression of scoliosis, studies have shown that bracing can produce a negative impact on the patient’s function, self-esteem, and body image, ultimately leading to diminished patient compliance as well as contributing to subsequent psychological concerns.8,9,10
In many cases, surgical intervention can correct neuromuscular scoliosis before secondary complications occur. Although improvements in surgical technique have decreased the invasiveness of corrective spinal procedures, research has shown that surgical spinal fusion is still associated with major complications including reduced spinal mobility,11,12 which is a significant concern for the SCI population due to their already impaired mobility. Loss of spinal flexibility can cause pain, discomfort, and loss of function that can place further dependence on caretakers for assistance with transfers and other activities of daily living. Spinal fusions are performed routinely to correct spinal curvature from neuromuscular scoliosis in the pediatric population and have shown to improve quality of life and limit a life-compromising cardiopulmonary condition.13 However, there is limited research supporting spinal fusion for neuromuscular scoliosis in the adult tetraplegic population. Spinal surgery is an invasive intervention that includes potentially life-threatening risks such as infection, further damage to the spinal cord, pneumonia, blood clots, and other life-altering complications that may result in further disability.5 For some individuals, surgery can induce a detrimental psychological response and elicit fear of the pathology, as well as anxiety about the hospital, pain, and concerns of survival.13
A Non-Invasive Treatment Approach
A different approach for correcting spinal deformity from neuromuscular scoliosis was used with the patient studied for this report. The treating physical therapist recognized that the new-onset neuromuscular scoliosis likely had a new precipitating cause and was compounded by functional scoliosis. Neuromuscular scoliosis is a lateral deviation of the spine that occurs in the presence of asymmetric tone of the paraspinal musculature due to a neurologic impairment. The condition is frequently compounded by gravity. Functional scoliosis is the result of the force of gravity working on unsupported structures when gravity has a moment arm. Functional scoliosis will reverse in a supine position, where gravity is eliminated. Therapeutic seating may be used to stop progression of functional scoliosis in an individual who is a full-time wheelchair user. The intervention in this case was to eliminate the confounding functional scoliosis and then quiet the asymmetric tone that was creating the neuromuscular scoliosis. The authors suggest that restoring function and independence by this conservative approach allowed the individual to regain dignity and a sense of control in his life.
Method
The research question that guided this study was: What is the lived experience for an individual with tetraplegia with new-onset neuromuscular scoliosis? More specifically, how did this condition impact his function and quality of life? And, what was his lived experience of interactions with healthcare providers during this episode of care?
A phenomenological approach was used in this case study. Phenomenology is the study of consciousness or intent, deliberated from the first-person point of view. This philosophy is used to examine the ways a person associates meanings with a given experience.14 Our participant was not specifically selected for this study; rather, he selected the researchers to investigate his lived experience retrospectively to determine specific qualitative effects of his new-onset neuromuscular scoliosis compounded by his SCI. Our participant was compelled to share both the emotional turmoil of his experience and the successful outcome to provide research that will change the future approach to treating SCI individuals dealing with neuromuscular scoliosis.
Data Sources
Primary data sources included our participant’s journal, an in-person interview with the participant that was audio-recorded and transcribed, notes from direct observation in the participant’s home and place of work, and subjective comments recorded in physical therapy (PT) documentation. We conducted thematic analysis of all the text material. The order of analysis was that of: (1) the journal, (2) PT documentation, and (3) the interview transcript. During the interview the initial coding scheme of the researchers was validated by the participant. Subsequently, the text of the transcript was analyzed. All analysis was done first independently by each of two investigators reading and coding the text that was meaningful in relation to the guiding questions. The initial coding was followed by a discussion for consensus to identify themes. Quotations from the transcripts were collated under these themes and organized by a timeline of before, during, or after the conservative intervention period.
Participant Profile
Our participant was a 48-year-old male with C6 complete tetraplegia that was stable for approximately 30 years prior to new-onset neuromuscular scoliosis. Our participant maintained a personal journal for two years during the episode of his neuromuscular scoliosis that documented his thoughts, feelings, and frustrations with his secondary physical changes, including his physical appearance and pain. His primary care physician attributed the neuromuscular scoliosis to his being an older wheelchair-dependent individual; he was referred for a surgical consultation for spinal fusion to prevent the progression of the spinal curve. Our participant previously had a fusion to stabilize his cervical spine directly following his SCI and was appalled at the surgeon’s recommendation to place a spinal rod from thoracic vertebrae 4 to lumbar vertebrae 3.
Our participant was unwilling to accept that this was his only option and was determined to find someone to help him treat his scoliosis conservatively. Being an individual with long-term tetraplegia who works in the wheelchair industry, our participant independently sought a wheelchair seating specialist who also held the belief that scoliosis was not an inevitable secondary impairment after an SCI. The physical therapist recognized that the scoliosis was a new condition and believed it developed secondary to a new cause, which created increased and asymmetrical tone in his trunk. This asymmetrical tone caused misalignment in his sitting posture and, in turn, gravity exacerbated his deformity by compounding with functional scoliosis. Therefore, the seating specialist believed it was a treatable deformity, not a permanent, inevitable complication. A more thorough explanation of the seating intervention is published elsewhere, as is a quantitative analysis of the intervention process.15
Results
Five major themes regarding the lived experience of our participant before the conservative interventions took place emerged from our research. The themes identified were: (1) feelings of social isolation, (2) diminished productivity at work, (3) losing control of function, (4) decreased independence, and (5) negative mental status. Our participant recounted experiencing these emotions not in a linear fashion, but with some overlap and circuity.
Feelings of Social Isolation
Our participant reported that he was unable to comfortably socialize with family and friends:
I lost about a year and a half of comfortably socializing with family and friends. …I didn’t do as many activities, just didn’t want to, just wanted to go to bed when I got home.
Although his wife and children were supportive during this year and a half, they also felt the compounding effects of isolation. Our participant’s involvement in relationships with his family and friends were put on hold due to physical pain, exhaustion, or feeling uncomfortable socially.
Diminished Work Productivity
As the neuromuscular scoliosis and pain increased, our participant felt as if his productivity at work suffered. He also felt that his bad seating posture created a poor image and that potential clients would not want to conduct business with him.
Hard to put in the hours I needed to at work. …[P]hysical appearance is important to sell wheelchairs.
Lost Control of Function
Our participant was concerned about his posture creating a poor base of stability, therefore affecting his ability to manually propel his wheelchair and fully participate in activities of daily living. He reported his spasticity as being so intense that he felt as if he had to lean forward to prevent falling out of his wheelchair.
Decreased Independence
Our participant lost considerable independence due to his decreased level of function. He reported that he became increasingly reliant on his wife for activities of daily living that he had performed independently prior to developing the neuromuscular scoliosis.
[I]t was really hard on my wife because I would just need more help, I was in pain.
Negative Mental Status
In addition to the everyday stressors of life that he was dealing with, such as financially supporting children through college, home remodeling projects, and new work ventures, our participant began to feel distressed and hopeless over his intense pain, poor body image, low self-esteem, and feelings of guilt. He also felt he was a burden on his wife, which ultimately led to depression.
I was suppressing stuff a lot, I was really down and frustrated.
Positive Change
Positive change in all five themes was recognized in the data associated with completing the conservative intervention.
Social: “I am back to full social participation.”
Work: “I can put in a long day at work and I am not fatigued by pain.”
Function and Independence: “I am much more functional and happier; transfers are no longer a problem.”
Mental Status: “I am very satisfied with where I am right now.”
Discussion
The data collected in this study contains the lived experience of a high-functioning individual with tetraplegia and how he dealt with secondary neuromuscular scoliosis. Although the reaction to conservative treatment may have been different in another person, this participant’s motivation and drive to find a conservative treatment option was unique to his situation, due to his feelings of horror toward a surgical intervention. He felt that he was not being given a real choice and that he was not being listened to. Because of his pre-existing surgical fixation from his initial injury, a surgical intervention would have resulted in fixed rods placed along the majority of his spine to create a stable symmetrical spinal column. He believed that the rods would have prevented the spinal motion necessary for functional activities such as twisting and bending to get dressed, drastically changing his independence for the worse. Even in the predicament of loss of function due to the neuromuscular scoliosis and pain, he felt the offered solution to be considerably worse.
Limitations
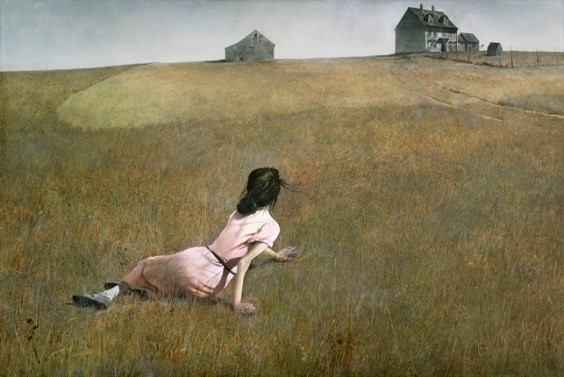
Because this story is retrospective, one may not be able to assume that our participant traveled through his emotions in the exact fashion presented; however, our participant’s report conveyed that as his function and independence decreased he developed a spiraling loss of self-esteem. It is evident in the photos captured of him prior to the start of therapy that our participant appeared to have given up on his self-image. He presents extremely disheveled, in sweatpants, with messy hair. Once the intervention is completed, he appears to take pride in his physical appearance with ironed slacks, collared shirt, and a symmetrical seated posture.
Our participant’s journals were limited in content and consistency, leading to gaps in reporting during the intervention period. Also, the in-person interview with our participant occurred more than a year after full correction of his scoliosis, which may have impacted the questions asked and our participant’s ability to recall facts and generate detailed responses to the interview questions. Nevertheless, the strength of this study is that the information is based within our participant’s lived experience in interactions with healthcare providers before, and during, the conservative intervention.
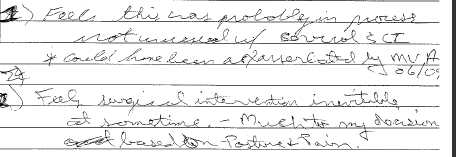
Detailed Review of the Participant’s Lived Experience
Our participant initially reported feelings about his inability to adequately perform his job duties. As an individual with tetraplegia working as a salesperson of durable medical equipment, specializing in wheelchairs, he felt his seated posture and physical appearance were vital to his credibility as a salesperson. If he did not appear physically functional, a client might look elsewhere for a wheelchair. In one of his many attempts to seek relief, he had a customized seat-back system installed in his manual wheelchair; however, he was further frustrated by the functional limitations of the system without resolving his other issues. He also resorted to using a power wheelchair when his pain and fatigue prevented him from functioning in his manual wheelchair. He was seeking something other than what was being offered by his healthcare providers, who continued to voice the belief that his duration of SCI would bring secondary complications that simply needed to be managed. The notes in his journal following a meeting with the orthopedic surgeon report that the physician told him new-onset neuromuscular was “not unusual with cervical SCI” but could have been “exacerbated by the MVA (a recent motor vehicle accident),” and that surgical intervention was “inevitable.”
When our participant met with the seating specialist, he described feelings of hopelessness and depression. The seating specialist took the time to listen to his concerns, understood how he was affected psychologically, and experimented with a treatment protocol that resulted in a successful outcome.
Central to the difference in this interaction was the listening. The participant relayed that he had been in a motor vehicle accident and he thought it might have contributed to this new problem. However, he had gone for imaging and there was no sign of fractures; his physicians did not see any connection. The seating specialist did not see new-onset neuromuscular scoliosis as inevitable, nor even expected, and therefore took the approach of investigating why it had occurred now, rather than just treating its presentation. The distress of the patient was acknowledged and understood, and some immediate relief for functional difficulty was offered as well by temporarily configuring his wheelchair for more trunk stability and accommodating postural asymmetry.
The exact cause that triggered the neuromuscular scoliosis is still unknown; however, the seating specialist hypothesized that it was due to the pull of asymmetrical muscle tone. This tone was presumed to be driven by a noxious stimulus, secondary to the recent motor vehicle accident. Despite the cause, once the tone developed and the malalignment was established, the lateral deviation became accentuated and perpetuated by gravity, pulling our participant into more significant spinal curvature and causing severe pain and decrease in function. Reversal of the negative psycho-social spiral began with listening, acknowledging, and then problem-solving in a collaborative manner.
Summary and Conclusion
This study offers a critical description regarding the lived experience of dealing with the psychosocial implications of the development of new-onset neuromuscular scoliosis in an individual with chronic SCI. Our participant described the process of his downward spiral, developing feelings of loss of control that resulted in hopelessness and depression. His feeling of loss of control was a product of repeated instances of medical specialists presuming his condition to be an inevitable progression of his SCI and ignoring his requests for an alternative to surgical intervention. However, once he began the conservative treatment process with the seating specialist, he reported regaining self-esteem and an improved body image, as well as a sense of regaining control of his life.
Qualitative information based within the individual’s actual lived experience through neurologic injuries and treatment is limited in the literature. Additional research should be conducted to further analyze the themes extracted in this study to increase the generalizability and applicability to all patients with secondary neuromuscular scoliosis. Based on the results reported in this study, treating clinicians should emphasize the individual patient’s goals, expectations, and beliefs regarding causation, be unafraid to explore various treatment protocols, and consider the psychological implication of all impairments.
Acknowledgements
The author would like to thank our participant for his time and commitment to this project so that this research can benefit others in similar situations in the future. This work is based upon a project completed by Christine Baniewich and Cedar Levine as part of their DPT education at the University of Puget Sound; the author was the treating clinician. We would also like to acknowledge our peer reviewers.
References
- National Spinal Cord Injury Statistical Center, Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham, 2016.
- Bernhard M, Gries A, Kremer P, Böttiger BW. Spinal cord injury (SCI) – prehospital management. Resuscitation. 2005;66(2):127–139.
- Burke DA, Linden RD, Zhang YP, Maiste AC, Shields CB. Incidence rates and populations at risk for spinal cord injury: a regional study. Spinal Cord. 2001;39(5):274–278.
- Zdanowicz N, Lepiece B, Tordeurs D, Jacques D, Reynaert C. Predictability of levels of physical and mental health in adults and adolescents: a 2 years longitudinal study. Psychiatria Danubina. 2012;24:9–13.
- Goodman CC, Fuller KS. Genetic and developmental disorders. In: Pathology: Implications for the Physical Therapist. 3rd ed. Louis, MO: Saunders/Elsevier; 2009;1108-56.
- Obid P, Bevot A, Goll A, Leichtle C, Wülker N, Niemeyer T. Quality of life after surgery for neuromuscular scoliosis. Orthop Rev. 2013;5(1):e1.
- Mulchey MJ, Gaughan JP, Betz RR, Samdani AF, Barakat N, Hunter LN. Neuromuscular scoliosis in children with spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19(2):96-103.
- Maruyama T, Grivas TB, Kaspiris A. Effectiveness and outcomes of brace treatment: a systematic review. Physiother Theory Pract. 2011;27:26-42.
- Rivett L, Rothberg A, Stewart A, Berkowitz R. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathic scoliosis: a comparative study. BMC Musculoskelet Disord. 2009;10:5.
- Vasiliadis E, Grivas TB, Gkoltsiou K. Development and preliminary validation of Brace Questionnaire (BrQ): a new instrument for measuring quality of life of brace treated scoliotics. Scoliosis. 2006;1:7.
- Master DL , Connie PK, Jochen SH, et al. Wound infections after surgery for neuromuscular scoliosis: risk factors and treatment outcomes. Spine. 2011;36(3):E179-185.
- Master DL, Son-Hing JP, Poe-Kochert C, et al. Risk factors for major complications after surgery for neuromuscular scoliosis. Spine. 2011;36(7):564-571.
- Kiecolt-Glaser J, Page G, Marucha P, MacCallum R, Glaser R. Psychological influences on surgical recovery: perspectives from psychoneuroimmunology. Am Psychol. 1998;53:1209-1218.
- Moran D. Introduction to Phenomenology. London, England; New York, NY: Routledge; 2000.
- Hastings JD, Dickson J, Tracy L, Baniewich C, Levine C. Conservative treatment of neuromuscular scoliosis in adult tetraplegia: a case report. Arch Phys Med Rehabil. 2014;95(12):2491-2495.




 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT