Mind Mapping: Using Visual Thinking to Improve Patient Care and Quality of Life
By Phillip Kellogg, SPT and Alli Nogi, PT, DPT
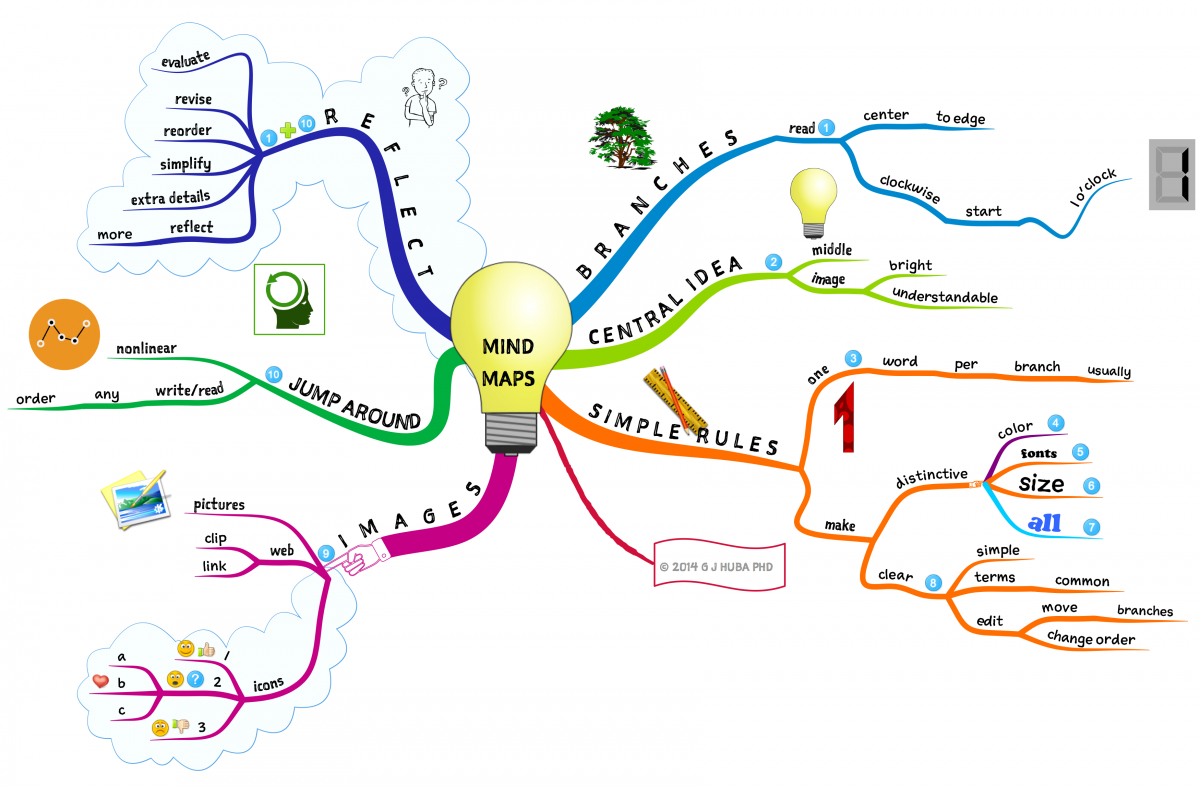
Figure 1. How to Mind Map: Demonstration of Text vs #Mindmaps in Instruction. This copyrighted mind map image is used with the permission of the author, Dr. George Huba. Click here to enlarge.
“When I open the map back up I can look at it for 10 seconds or less and know immediately what I was doing and recover my train of thought. That is, I can LOOK AT IT… I really do not know what to make of it but I do believe that this is very important and illustrative of how the demented or healthy brain is adapting to other information channels using cognitive reserve and brain plasticity… I forget but I remember and that maintains a creative process.”
—Dr. George Huba
The ability to effectively perceive, synthesize, and share information may go unnoticed or undervalued in the day-to-day lives of most people. Yet its importance never diminishes, and is made ever more apparent for those coping with impacted or declining cognition. Individuals undergoing rehabilitation or living with a disability share a common need for finding ways to better manage their individual cognitive demands. From the initial work of Professor Tony Buzan to the ongoing contributions of Dr. George Huba, the concept of mind mapping has developed as a tool to help countless individuals better process information.
This article presents the principles of mind mapping as originated by Professor Tony Buzan, and describes Dr. George Huba’s journey from an initial diagnosis of dementia through his contributions to mind mapping, which have served to improve his own quality of life and that of others. It concludes with a report on the potential impact of mind mapping on patient care and quality of life.
An Emerging Tool for Empowerment
Research is showing that mind mapping may serve to further augment clinical practice guidelines to help improve independence in people with dementia.1 Dr. George Huba’s work has highlighted how mind mapping may serve as an empowering tool for such populations; mind mapping has gained recognition as a tool social workers and caregivers can use to help people with dementia maintain quality of life.2 Yet, there continues to be limited application of mind mapping within the rehabilitation field. There is a need to investigate the multifaceted nature of mind mapping, and its potential applications. For instance, could the effects of mind mapping for those with impacted cognition stem from its ability to help them satisfy such psychological needs as autonomy and competence, which are essential to “healthy cognitive, behavioral, and social functioning”?3 In clinical psychology, the importance of addressing psychological needs is acknowledged in Self-Determination Theory, which argues that a person’s intrinsic or self-sustaining motivation to choose healthy behaviors depends on the ability of providers to support an individual’s sense of choice and their self-efficacy.4
Dr. Huba’s Journey
Take a moment to imagine you are working as a research methodologist evaluating and developing mental and social healthcare programs for underserved populations. You are good at what you do; in fact, you are an expert whose professional experience crosses the fields of neuroscience research, patient care, aging, and healthcare systems development.
Now imagine that after 35 years of research and helping others, you begin to experience your own cognitive difficulties. Simple daily tasks, planning your schedule, learning new information, communicating with others, and navigating social situations transform into stressful chores and become physically and mentally more difficult than what you might expect. Eventually, these difficulties are confirmed to be the result of a progressive neurodegenerative disease, diagnosed ultimately as the combination of frontotemporal dementia (FTD) and Parkinsonism, which has no proven medical cure and leads to cognitive and physical decline. What would you do next?
Facing the Crossroads. More than a hypothetical example, the scenario depicted above is a simplified description of the challenging crossroads Dr. George Huba faced when FTD/Parkinsonism began affecting his health, as depicted in his mind map, I Refuse to “Suffer” with Dementia. Despite the overwhelming nature of Huba’s diagnosis, his determination to continue living purposefully and to contribute to his and potentially others’ well-being remained. Empowered by his 35 years of experience in psychology research, Huba saw his retirement in 2011 not as the end, but as a transition in his career journey that would lead him toward investigating cognitive strategies and visual thinking tools that might help him and possibly others living with dementia.5
Powered by his understanding of the scientific method, Huba’s proactive problem-solving catalyzed newfound hope through innovation at a time in his life when hopelessness might have been the expected result. Being diagnosed with a progressive neurodegenerative disease may feel like a “dead-end road,” and perhaps for some it is treated as such; however, Huba’s questioning of this fate, and his pursuit of living well, exemplify the human potential that still exists even when faced with a dire prognosis.
Using Visual Thinking. Huba’s training in psychology and his passion for inquiry enabled him to enhance his own quality of life and demonstrate the effectiveness of “visual thinking”—the phenomenon of using images and graphic design to facilitate cognitive processes. He has shown how the visual-cognitive technique of mind mapping can foster self-empowering methods by which a person may “live well with dementia.” Interpreted through the measured lens of a scientist, Huba’s journey and discoveries are chronicled and continually updated on his blog, Hubaisms. His willingness to share the blog’s content and communicate possible solutions to others with dementia has allowed anyone interested to benefit from his personal experimentation and research with these tools. Although his blog is still the definitive source of his discoveries, he has also published the e-book, Mind Mapping, Cognitive Impairment, and Dementia (Huba’s Bolero), which presents some of these discoveries and explores the integration of mind-mapping theories and practice.6
Huba does not claim that mind mapping is curative for dementia or that it affects everyone equally. Yet, the technique has undoubtedly provided him and others a low-cost and impactful strategy for improving cognitive functioning and quality of life. Although his training in psychology and research surely added to Huba’s expert use of mind mapping, it is a technique that can be accessible to people of varying professions and educational backgrounds, and can be simplified into a few basic principles.
Basics of Mind Mapping
Mind mapping is essentially a visual-thinking tool that is adaptable to any particular population or setting, and can be utilized by anyone who follows its basic principles to effectively organize information.
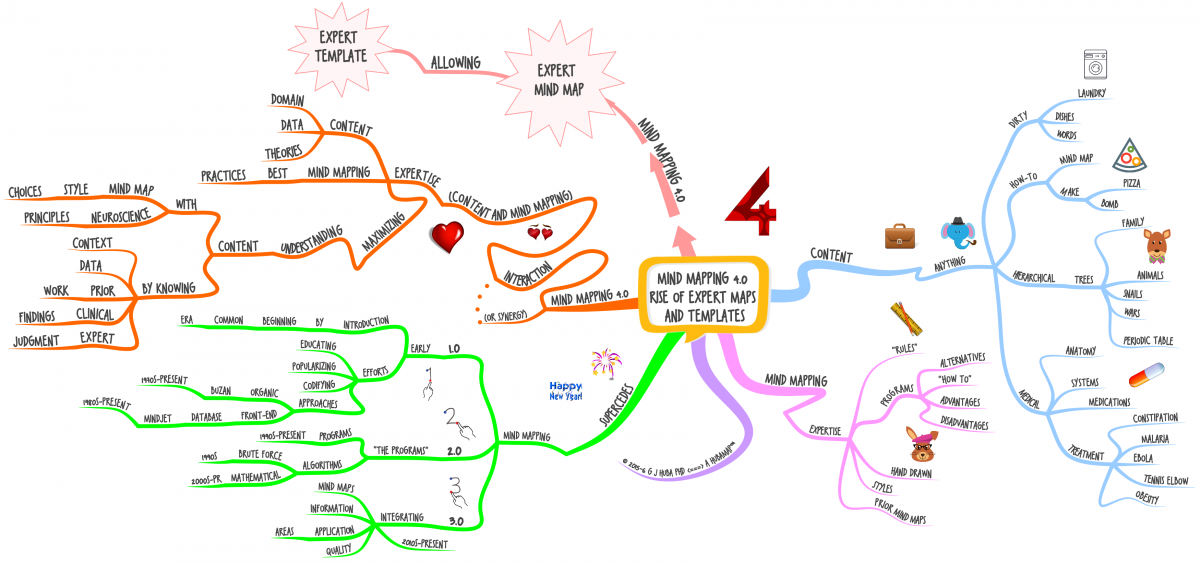
Figure 2. #MindMapping 4.0: The Era of Expert #MindMaps and Templates. This copyrighted mind map image is used with the permission of the author, Dr. George Huba. Click here to enlarge.
As Figure 2 shows, a mind map focuses on presenting information in a diagrammatic format with a core idea in the center branching into differentiated details using visually stimulating strategies to help draw in the viewer’s attention.
- The differences in line shape, color, and pictorial icons help trigger a person’s recall by developing different visual associations and delineating where concepts diverge.
- Additional sub-branches provide details and illustrate the interconnectedness of information, as well as how a concept can be rooted in different yet interrelated parts.
- Often read clockwise starting from “1 o’clock,” the maps allow the reader’s eyes to skip from one point to another within the map and use the different levels of branching to find information efficiently.
Within this framework, users can tailor their mapping toward any subject—whether that be organizing a “To-Do List” of daily activities, or outlining a patient’s treatment plan.7 Mind mapping can be simplified into an accessible format, as will be discussed here; higher levels of expert formatting can be used to enhance the way professionals in specific fields access and integrate knowledge.
Development of Mind Mapping
The growth of mind mapping from version 1.0 to what Huba’s map describes as Mind Mapping 4.0 (Fig. 2) has occurred through the development of its basic principles leading to its formatting into computerized programs, its integration as a theoretical method, and its optimization for expert and individualized use. This journey has required the contribution of developers whose work is described in more detail in posts such as this one in his blog, Hubaisms.8
Professor Tony Buzan’s original development of Buzan-style organic mind mapping and the iMindMap computer program have been influential in creating and defining the foundational elements of mind mapping as a unique, critical, visual thinking tool.
Building upon Buzan’s contributions, Huba’s research, presented in his Integrated Theory of Mind Modeling (Mind Mapping), provides a comprehensive articulation of mind-mapping concepts, describes elements of the highest-quality maps, and defines the characteristics of Huba’s own MindModelTM approach.8
Mind Mapping 4.0 may provide an innovative means of optimizing information processing for its users, whether they be patients/clients or healthcare professionals.8 The impacts of these developments and the dissemination of mind mapping have yet to be fully realized; however, its impact on two major areas described below—patient quality of life and patient care—suggests exciting opportunities for other innovators to investigate its adaptive utility.
Patient Quality of Life
Caring for people with dementia is one area where mind mapping has gained a great deal of attention. The stigma of dementia—that of the condition being equated with hopelessness and reduced autonomy—is being challenged by Huba, and by those social workers, caregivers, and people with dementia who have found mind mapping to be an effective tool for facing the challenges of neurocognitive decline in order to maintain a better quality of life. How exactly mind mapping uniquely engages a person’s cognition is, to date, not well-defined; however, the impact of its use as documented by Huba demonstrates its value. In #MindMapping with #Dementia: Me and My #MindModels, Huba shows how this process allows him to exercise an understanding, recall, and creativity that feels similar to those processes he experienced before the onset of his neurodegenerative condition.
Visual Comprehension. Huba describes in his blog how he can be working on his computer completing a map, leave his desk, and forget the work he was doing. However, he notes, “When I open the map back up I can look at it for 10 seconds or less and know immediately what I was doing and recover my train of thought. That is, I can LOOK AT IT,” and understand.9 This visual comprehension and recall appears to effectively vary from other forms of comprehension that may be disrupted for a person with dementia. While admitting that this mechanism for thought recovery is not entirely clear to him, Huba does suggest that it may be “illustrative of how the demented or healthy brain is adapting to other information channels using cognitive reserve and brain plasticity.”9
Although research exploring such theories in relation to mind mapping is still limited, evidence showing experience-dependent brain plasticity persisting into older age, and cognitive reserve reducing rates of cognitive decline may offer preliminary support for exploring such neurological mechanisms.10,11
A Focus on What Does Work. Huba’s work with mind mapping presents a crucial shift in perspective regarding dementia—away from thinking first of those structures that have degenerated, to instead exploring those that are still intact, capable of growth, and offer a physical and malleable source of hope. The stress that develops from the cognitive challenges of dementia can lead to a downward spiral that prompts people to disengage with others and to retreat from the activities that bring them happiness. Mind mapping does not fix the underlying neurological mechanisms of dementia; however, it can act as an effective tool to help people with dementia carry out those fundamental cognitive processes that are being disrupted. This may empower an individual to better engage in a treatment plan, organize daily activities, interact with others, and navigate away from feelings of anxiety, hopelessness, or depression. Overcoming the debilitating emotional impacts of dementia, and facilitating confidence and creativity, may help reduce the sequelae of progressive neurocognitive decline. Mind mapping can thus support individuals in their refusal to suffer from dementia and help them find a new path to living well.
Patient Care
As Huba’s map in Figure 3 illustrates, mind mapping is considered to have a multitude of purposes in patient care. These range from helping providers communicate with patients/clients and their families, to clarifying how information is processed and shared among healthcare professionals.
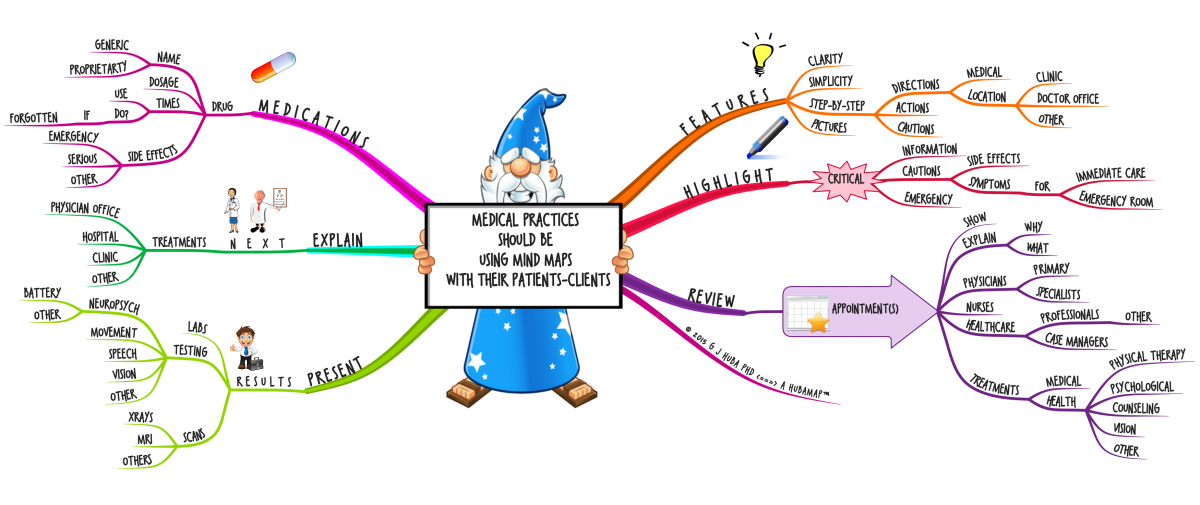
Figure 3. Medical Practices Should Be Using #MindMaps with Their Patients. This copyrighted mind map image is used with the permission of the author, Dr. George Huba. Click here to enlarge.
In relation to teaching and learning, mind mapping may help improve health literacy for patients who are overwhelmed by health information, struggling with reading comprehension, or dealing with a cognitive condition such as dementia. Using mind maps with patients can serve as a tool for healthcare providers to help patients better understand their treatment plans, and act as a guide for the patient to reference for self-care and self-advocacy. It may also act as a helpful resource for healthcare professionals to organize and integrate a client’s health information, as demonstrated by the map in Appendix 1, and help family and caregivers better understand a loved one’s needs and impairments.
Mind Mapping and Physical Therapy. Clinicians who wish to explore mind mapping can now follow the lead of others who have identified ways that mind mapping can be integrated into the physical therapy plan of care and treatment sessions. Clinicians use mind mapping to open conversations with clients about how their impairments influence their ability to access their community and achieve their goals. During conversations or as a treatment session dual task, the clinicians guide clients in creating their own individualized mind maps (Fig. 4, Appendix 2). The guidance provided utilizes the main categories of the International Classification of Function, Disability and Health (ICF) model, insuring that the patient’s impairments, participation restrictions, and environmental and social influences are addressed. The process proceeds as follows:
- Starting with the patient’s name, condition, or goals in the middle of the map, clients are first asked to write, or verbalize, their chief medical diagnosis.
- From their medical diagnosis, they are asked to add branches of their perceived impairments, like decreased muscle strength, decreased balance or coordination, and their perceived barriers, such as certain fears or social and environmental factors.
- After identifying these impairments, clients are then guided on why these aspects are important, allowing them to develop connections between the impairment and their inability to complete a task. The inability to complete a functional task may be further linked to how this impacts their ability to participate in a community setting.
- Specific therapeutic exercises that need to be completed in the clinic and within the home setting are listed and connected to impairments, allowing clients to see the importance of their treatment and home-exercise programs, and how they will help them reach their rehabilitative goals in a safe and effective way.
Additionally, this process allows clinicians to realize the patient’s understanding of their disability and the rationale of treatment, and offer patient education. Clinicians can further use this as an opportunity to support a patient’s autonomy as the patient voices their concerns and revisits what it is they truly want to accomplish in their rehabilitative journey.
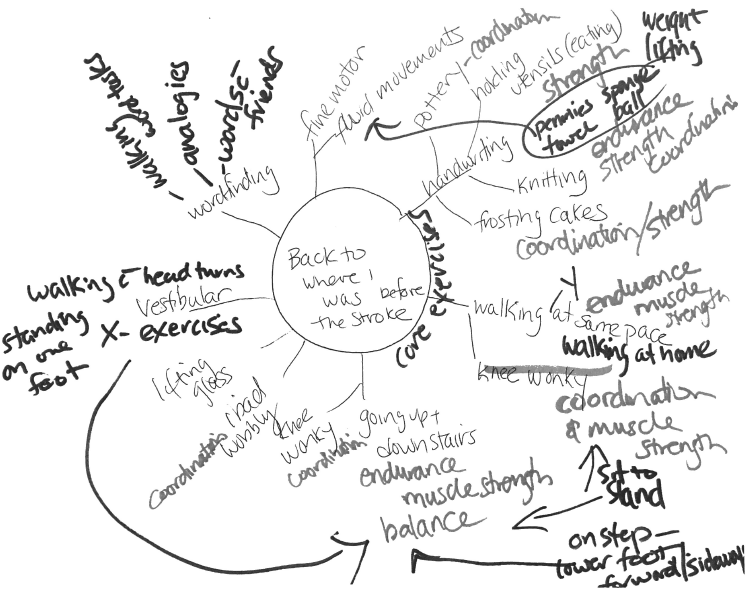
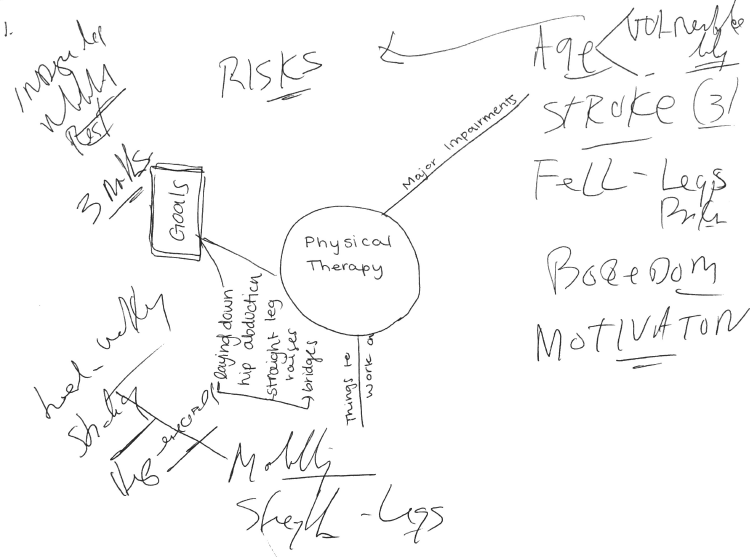
Figure 4. Example of a Patient Mind Mapping Their Physical Therapy Rehabilitation. Mind Map image created by and contributed with the permission of an Outpatient Neurological Rehabilitation Clinic patient. Click here to enlarge.
In practice, mind mapping can stimulate greater patient engagement, providing an opportunity for the clinician to offer additional education regarding rehabilitation, and spark new directions within the rehabilitative plan of care. Even without sophisticated computer technology or mind-mapping software, a version of mind mapping can be implemented with pen and paper during physical therapy sessions, allowing clients to visualize how their impairments link to functional activities, and how physical therapy interventions and home-exercise programs can optimize rehabilitation.
Clinician Guidelines. Clinicians starting to use mind mapping with their clients may wish to refer to Buzan’s 7 Steps to Making a Mind Map, which offers introductory guidelines for formulating an effective mind map.12 As clinicians gain familiarity with the process, they may review the variations in approach offered by Huba throughout his blog Hubaisms, as they tailor their or their clients’ mapping to better serve individual needs.
Future Directions
Mind mapping has the potential to impact healthcare outcomes and the quality of patient care by visually depicting and organizing information into accessible and engaging formats. Further research needs to be completed to investigate mind mapping’s neurocognitive impact, and the differences between mind mapping and other cognitive aids. Mind mapping may additionally have the capacity to improve patient motivation during the rehabilitative journey, and improve overall quality of life as it helps involve patients in their plan of care and develop strategies for coping with cognitive deficits. It is imperative that the rehabilitation community further investigate mind mapping, to fully understand its potential and optimize its usage for patient care.
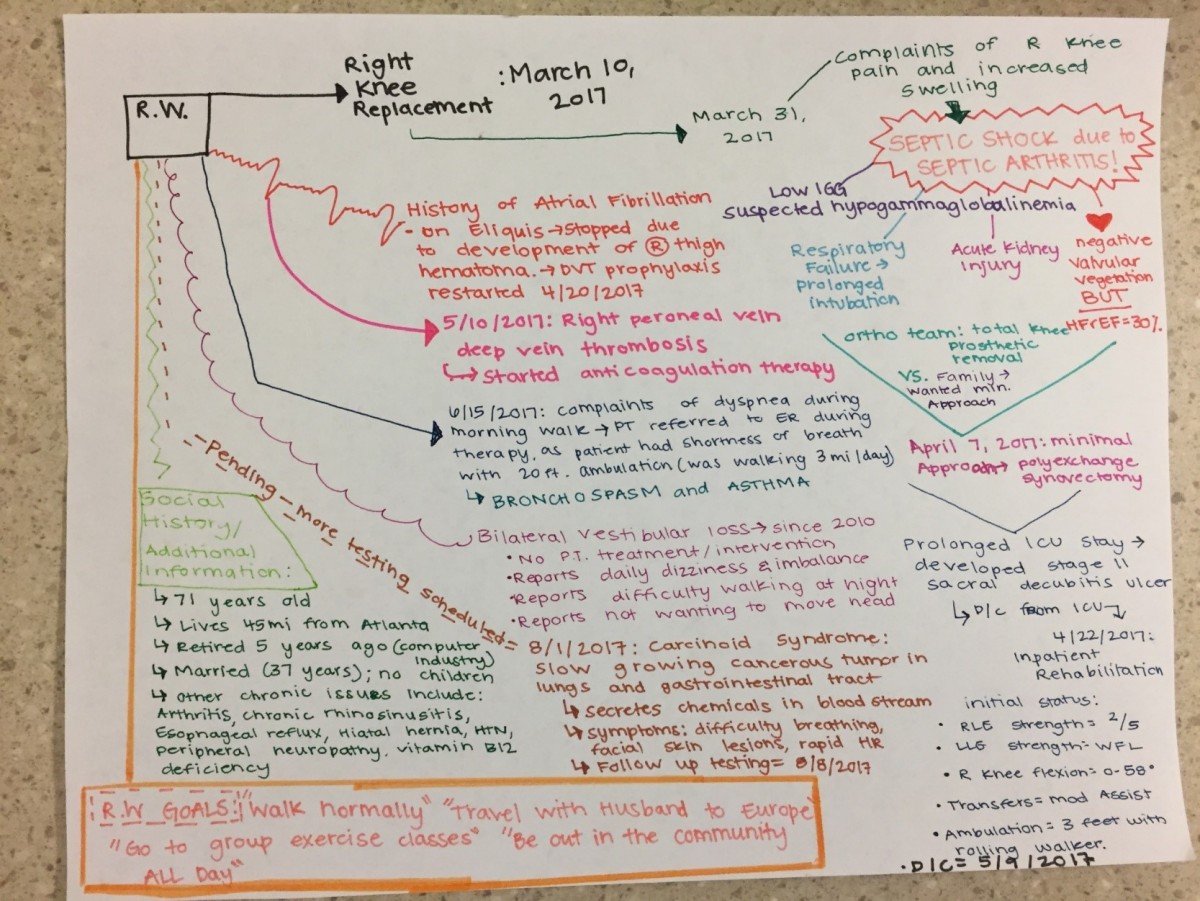
Appendix 1. (Author: Dr. Allison Nogi. Patient Case Integration).
Appendix 2. Example of Physical Therapist-Guided Patient Mind Map.
Mind Map image created by and contributed with the permission of an Outpatient Neurological Rehabilitation Clinic patient.
Acknowledgements
The authors and JHR Editorial staff would like to extend our sincere gratitude to Dr. George Huba for his thoughtful support and wise guidance in the development of this manuscript and for generously sharing the images of his mind maps. His pioneering work in mind mapping and his engaging blog (https://hubaisms.com) offer a unique and innovative approach to visual thinking methods to increase the quality of care and quality of life for individuals with dementia. Thank you for reminding us that “Every life is priceless and every gain is huge.” (https://hubaisms.com/2012/09/)
References
- Dyer SM, Laver K, Pond C, Cumming R, Whitehead C, et al. Clinical practice guidelines and principles of care for people with dementia in Australia. Australian Family Physician. 2016;45(12):884-889. PMID: 27903038.
- Michaeli D. Dementia care: use mind mapping to improve quality of life. Social Work Career Website. January 19, 2017. Available at: http://www.socialwork.career/2016/03/dementia_mind_map_improve_quality_of_life.html. Accessed August 1, 2017.
- Niemiec CP, Ryan RM. What makes for a life well lived? Autonomy and its relation to full functioning and organismic wellness. In: David S, Boniwell I, Conley Ayers A (eds.) The Oxford Handbook of Happiness. Oxford, UK: Oxford University Press; 2013:214-226.
- Williams GC, Niemiec CP, Patrick H, Ryan RM, Deci EL. The importance of supporting autonomy and perceived competence in facilitating long-term tobacco abstinence. Ann Behav Med. 2009;37:315-324.
- Huba, GJ. My life as an ongoing cognitive and “medical” experiment, #MindMap. Hubaisms. January 5, 2016. Available at: https://hubaisms.com/2016/01/05/my-life-as-an-ongoing-cognitive-and-medical-experiment/. Accessed August 1, 2017.
- Huba, GJ. Mind Mapping, Cognitive Impairment, and Dementia (Huba’s Bolero). Chapel Hill, NC: ABCXYZ LLC; 2015. Available at: https://www.amazon.com/Mapping-Cognitive-Impairment-Dementia-Bolero-ebook/dp/B00UP3Q2ZY. Accessed August 1, 2017.
- Huba GJ. How to mind map: demonstration of text vs #MindMaps in instruction. Hubaisms. January 25, 2014. Available at: https://hubaisms.com/2014/01/25/demonstration-of-text-vs-mindmaps-in-instruction/. Accessed August 1, 2017.
- Huba, GJ. #MindMapping 4.0: The era of expert #MindMaps and templates. Hubaisms. November 10, 2016. Available at: https://hubaisms.com/2015/11/10/httm-2016-1-mindmapping-4-0-the-era-of-expert-mindmaps-and-templates/. Accessed August 1, 2017.
- Huba GJ. I do not know what to think about my process of creating #MindMaps while having major neurocognitive disease (#Dementia). Hubaisms. July 18, 2016. Available at: https://hubaisms.com/2016/07/18/what-to-think/. Accessed August 1, 2017.
- Lövdén M, Bodammer NC, Kühn S, Kaufmann J, Schütze H, et al. Experience-dependent plasticity of white-matter microstructure extends into old age. Neuropsychologia. 2010;48(13):3878-3883. doi:10.1016/j.neuropsychologia.2010.08.026.
- Hindle JV, Martyr A, Clare L. Cognitive reserve in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2014;20(1):1-7. doi:10.1016/j.parkreldis.2013.08.010.
- Buzan T. 7 Steps to making a mind map. Tony Buzan Mind Mapping. Available at: http://www.tonybuzan.com/about/mind-mapping/. 2011. Accessed August 1, 2017.



 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT