Editorial: Strange Bed-Fellows: Can the Humanities Help the Electronic Health Records Problem?
By Sarah R. Blanton, PT, DPT, EDITOR-IN-CHIEF
“Time, sympathy and understanding must be lavishly dispensed, but the reward is to be found in that personal bond which forms the greatest satisfaction of the practice of medicine. One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”
[Excerpt from a speech given by Francis W. Peabody, MD, to medical students at Harvard University, October 21, 1926.]
I was recently intrigued by a New York Times Opinion piece by Theresa Brown and Stephen Bergman entitled: “Doctors, Nurses and the Paperwork Crisis That Could Unite Them.” They aptly describe the required use of the electronic health record (EHR) system as “a pernicious problem that drives so much of our [clinicians’] mutual discontent.” With the passage of the 2009 Health Information Technology for Economic and Clinical Health Act, the use of the EHR was originally intended as an innovative approach to improve healthcare quality and efficiency. Yet today, clinicians are consistently pulled away from interactions with their patients to engage with the demands of these not-fit-for-purpose technologies.
EHR systems, notorious for poor user interfaces with inadequate usability, are now causing the “4,000 clicks” quandary. In a study of emergency-room physicians, researchers found that over the course of a busy 10-hour shift, the mean percentage of clinical time spent on data entry was 43%, as compared with only 28% of time spent in direct patient contact, with nearly 4,000 mouse clicks recorded. Melnick and colleagues found in a cross-sectional survey that American physicians gave EHR technologies a grade category of ‘F’ compared to other current technologies’ usability. What is even more concerning, the researchers found a strong dose-response relationship between EHR usability and risk for physician burnout.
The National Academy of Medicine has published a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-being,” confirming that clinicians spend fully half of their days interacting with the screen instead of the patient, concurring that this immense documentation burden is a primary contributor to clinician burnout.
Where do the humanities fit into this complex and broad-reaching issue? First of all, a humanities perspective helps us see that the core issue is not simply the frustration caused by the dysfunctional check-boxes or the poor metrics of technical usability. It helps us focus on how these factors negatively impact our relationship with our patients—and ourselves. The true value of our work lies in the shared meaning-making we experience during our clinical encounters; the disconnect arises when de-humanization occurs as a result of our requisite divided attention. Not only are we separated from our patient’s story; we also risk our own story, our reason for choosing healthcare as a profession. As Dr. Ron Epstein notes in his book Attending, the industrialization of medicine erodes our sense of self because we can no longer practice in a manner consistent with our values.
Secondly, exploration in the humanities is characterized by interdisciplinary approaches seeking creative innovation. Solving the problem of a dysfunctional EHR system will take more than the development of more advanced computer technologies. Truly solving complex problems such as these necessitates pulling wisdom from a broad range of disciplines. Recognizing that EHR is not just a function of technology and data, but also of policy, politics, law, and business, shows us that a solution must be found beyond pure science and engineering-based approaches. For instance, how can legislative policy alone inform the efficient flow of clinically meaningful information that supports novel ways to approach problems of health disparities? How does economic theory alone help us step out of a narrow focus on health data to a broader understanding of the financial drivers of healthcare that influence implementation practices?
The humanities help us recognize that our focus must begin with developing more human-centered approaches, from the societal level down to the individual, personal level. For example, solutions that pull from the arts that engage visual-design strategies can guide the individual user experience with ERH. Having a fluency in the language of art history—such as understanding how the formal elements of light, color, lines, and space interact to create composition in paintings, or how meaning is communicated through images—can fuel innovative perspectives that view interactions with a computer monitor in similar ways that we see movement in classic works of art. Could these more humanized electronic platforms not pull us away from our patients, but perhaps even facilitate our communication and connection with them? What would it look like if the patient actually co-created that record with us? The founder of the Columbia Narrative Medicine Writing Program, Dr. Rita Charon, does precisely this, using skills of narrative medicine to write collaboratively with her patients to ensure an accurate medical history-taking.
Thirdly, the humanities offer a space for critical inquiry, pushing us to ask: “Why are things the way they are?” Learning lessons from critical theory and disabilities studies, how do we create spaces to challenge normative assumptions that bind and dampen creative solutions? Barbara Gibson, PhD, comments on how the role of critical perspectives in rehabilitation can easily be applied to the use of healthcare Internet technology (IT):
“Critical thinkers utilize theories from the social sciences and humanities to consider the underlying assumptions, understandings, and contexts behind [rehabilitation] practices. There are many different critical perspectives (including for example, post-modernism, feminism, critical disability theories, new materialism, and post-colonialism) that can be utilized to interrogate and inform [rehabilitation] practices. All share a consideration of the socio-political aspects and cultural contexts informing care, and work to illuminate the assumptions that underpin health practices and their hidden or less obvious effects on recipients of care… Research and scholarship employing a critical approach work toward creating unanticipated opportunities to think and do [rehabilitation] differently. They offer ways to consider deeply why practitioners do what we do, and to highlight the intended and unintended effects of practice-as-usual. The aim of critical work is to build more ethical, inclusive, and equitable healthcare practices. As such, they complement the humanities and the arts with their shared aims of challenging reductive, linear, and/or evidence-based modes of thinking that dominate the [rehabilitation] sciences.”
Perhaps policy makers did not anticipate the consequences of clinician burnout from the EHR implementation; however, the continued lack of critical inquiry perpetuates this progressive erosion of the clinician psyche.
Coming back to the NY Times Opinion piece, Brown and Bergman note that:
“Part of the reason for inaction is that not enough clinicians are making it loud and clear that change is necessary. Doing so requires a unified voice across our professions—and unfortunately, right now, doctors and nurses are anything but unified.”
I underscore the critical role of working together across disciplines to drive the societal and policy changes that must occur to fully capitalize on the positive potential of healthcare IT. Yet, while it is perhaps a symptom of the greater problem of healthcare silos, these authors only mention physicians and nurses. Lamenting the lack of a unified voice, I say, what about other healthcare professionals such as rehabilitation therapists? Perhaps if we recognize the problem of EHR in the context of broader issues of social justice and inequities in healthcare we can harness the power of activism to truly unite across professions to solve the “4,000 clicks” problem. Indeed, health systems that are authentically patient-centered have the potential to help us as clinicians re-imagine our sense of purpose in work, fostering humanism (humanitarianism) in that re-connection with our patients.
Our Spring 2022 issue of JHR offers us opportunities to sit in that space of humanities for critical reflection and exploration. The articles and essays include:
Viral Imaginations: Healing Through Pandemic Narratives
By Michele Mekel, JD, MHA, MBA and Lauren Stetz, PhD Candidate, MA
As the COVID-19 pandemic blindsided us in 2020, an interdisciplinary team at The Pennsylvania State University (Penn State) developed the Viral Imaginations: COVID-19 project to encourage all Pennsylvanians to creatively cope by telling their unique stories. The results, sampled here, were profound. The authors note that similar projects could “benefit healthcare, including rehabilitation, by creating understanding among and between patients, providers, and others involved in the circle of care.”
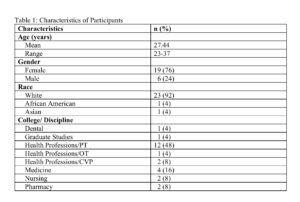
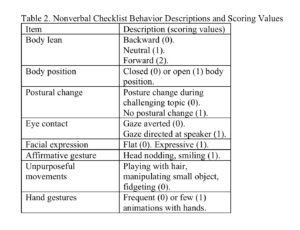
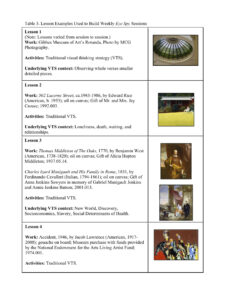
By Cynthia Dodds, PT, PhD; Brooke Mulrenin, OTR/L, MS; Lisa Kerr, PhD, Carrie Cormack, DNP, APRN; Kimberly Kascak, MS; and Rebecca Hiester, Director of Education and Programs, Gibbes Museum of Art
In a second article deeply exploring the insights of the Eye Spy program (see Eye Spy, 2018), Cynthia Dodds et al examine the effects of guided visits to an art museum on affective domain development and interprofessional perspective in health science students. The authors demonstrate, step by step, how using visual-thinking-strategy instruction in a museum setting can support the development of “compassionate and patient- and family-integrated care providers.”
By Sarah E. Luna, PT, DPT; Nathan Brown, PT, DPT; and Cynthia Dodds, PT, PhD
This article strives to encourage the use of humanities within physical therapy education and practice by offering examples of three health humanities-based instructional activities, including two implemented at US universities. “As curricular models in physical therapy education evolve,” the author notes, “the importance of humanities-based instruction to develop empathetic physical therapists should be considered and implemented, as it will not only benefit future patients, but the field of physical therapy as well.”
By Michele Slaton, PhD, and Brick Johnstone, PhD, ABPP
This poignant report maps the direct line between the introduction of humanities into rehabilitation and its powerful impact on healing—and beyond. It begins with a case study of a 47-year-old woman with a right temporal lobectomy at age 22, who has written poetry over the past 30 years “to express her positive mystical experiences.” The content then switches to the first-person, with poet Michele Slaton describing the remarkable insights she has experienced on her rehabilitation journey. Her poems, included here, present a deep and moving argument for the gifts that a physical crisis can unlock when humanities play a part in treatment.
JHR-CHEP Student Narrative Essay Winner
By Joseph Rivera, SPT
Congratulations to Columbia University Doctor of Physical Therapy Program graduate student Joseph Rivera, SPT, the winner of the 5th annual physical therapy student essay contest co-sponsored by the ACAPT Consortium for the Humanities, Ethics, and Professionalism (CHEP) and JHR! The judges described his essay, “Finding Voice and Vulnerability through Virtual Learning,” as “intriguing, thought-provoking, and courageous” as he draws insights from his Puerto Rico background to describe his journey to find his voice through the safety of Zoom enclosed dialogue. He highlights the intersection of power and privilege and the impact that virtual learning had on those discussions. Essays from the two additional finalists, Bridget Graff, SPT (Marquette University) and Noah Watson, SPT (A.T. Still University), will be published in the Fall 2022 issue of JHR.
Doing Healthcare Research Differently: An Introduction to SocioHealthLab’s Special Series, Part 1
By Rebecca E. Olson, PhD; Jenny Setchell, PhD, BScPT, Grad Cert (Clin PT); and Tim Barlott, PhD, MSc, Grad Cert (Community-Based Participatory Research), BScOT
In this first of two installments within SocioHealthLab’s special video series with JHR, the authors “begin doing health research dissemination differently” by telling their “story/stories” through animation, music, sound, and discourse. The videos shared here range from heart-rending personal patient experiences of pain and fear, to a humorous ‘what-if’ look at rehabilitation processes with the use of cartoon animals. Viewers are invited to relax and share these brief accounts in a “quiet space.”
“Afflicted With Wishes for Change”
By Dustin Willis, PT, DPT
In this powerful poem, Dustin Willis reflects on the frustration a parent feels while seeking answers and compassion from doctors who are limited in their ability to offer adequate time, thought, and care to his son’s complex needs. His reflections are a plea for change as he navigates our broken healthcare system- a heartfelt appeal that keeps needing to be made.
By Kirsten Woodend, RN, MSc, PhD
Kirsten Woodend considers the space between being “broken” and being “whole,” when the patient’s road to recovery will never end in full rehabilitation. She writes of the difficult struggle to choose between “acceptance” and constant striving toward “recovery.” In this poignant poem, she finds herself at a fork in this unique road.
By Sophie L. Schott
Inspired by reflections on the current Covid-19 pandemic and recalling American Medical Association debates over the “duty to treat” individuals with HIV and AIDS in the 1980s, Sophie Schott has crafted a poem that challenges us not to repeat history by refusing to treat marginalized patients. “History of Present Illness” questions whether clinicians should be guided by personal preferences or by a higher calling.
By Michele Mekel, JD, MHA, MBA
With observant humor and a brisk rhythm, Michele Mekel’s poem evokes the memory of an awkward encounter in a waiting room, where a doctor initially dismissed her at first sight. “Office Visit” serves as a reminder to healthcare professionals to be aware of tendencies to make snap judgments and underestimate their clients.
Resources to Promote Inclusion and Belonging
By Anjanette Nuñez, PT, DPT; DeAndrea Bullock, PT, DPT; and Sarah Caston, PT, DPT
For Spring 2022, the JHR is publishing for the first time a resource list related to cultivating belonging for students and patients in healthcare education and healthcare settings. This exceptional compilation of articles, books, movies, and artwork could serve as “an academic course in and of itself,” according to one of our editors.
Thank you for joining us. We hope you find inspiration in the Spring 2022 issue of JHR.
If you are interested in submitting your work to JHR, please review our Submission Guidelines. If you are considering being a reviewer, please contact Dr. Sarah Blanton: follow the Contact link, indicate the content area you are interested in reviewing, and attach your CV.








 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT